#15,444
Tomorrow, September 1st, marks the start of National Preparedness Month (#NPM), which has been promoted by FEMA, Ready.gov, and others (including AFD) since 2004. Each year, during the month of September, I double down on preparedness blogs in support of this campaign.
This year will be no different, although personally, the stakes have never felt higher.
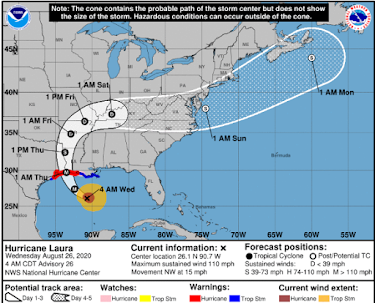
We are just now entering the height of hurricane season, in what has already been a record breaking year. The earth, and the United States in particular, has been in a major earthquake drought for years, and as we all know - droughts - even good ones, end eventually.
- When Category 4 Hurricane Harvey battered and flooded east Texas in 2017, it ended an 11+ year drought in major (CAT 3+) land-falling hurricanes in the Continental United States. Since then, we've seen Irma, Michael, and Laura.
- When a novel swine-origin H1N1 virus emerged in 2009, it ended a 40 year drought in flu pandemics, and just ten years later we have our 2nd pandemic.
Over the next couple of years, the sun will climb back towards solar maximum, putting the earth at risk of damaging solar storms (see USGS: Preparing The Nation For Severe Space Weather).
In 2014 a study was published suggesting the odds of earth being struck by one of these solar super storms is actually a lot higher than we’ve previously thought. From a NASA article:
In February 2014, physicist Pete Riley of Predictive Science Inc. published a paper in Space Weather entitled "On the probability of occurrence of extreme space weather events." In it, he analyzed records of solar storms going back 50+ years. By extrapolating the frequency of ordinary storms to the extreme, he calculated the odds that a Carrington-class storm would hit Earth in the next ten years.
The answer: 12%.
In 2018's NIAC: Surviving A Catastrophic Power Outage, we looked at the President's National Infrastructure Advisory Council (NIAC) report on the potential for a prolonged grid-down scenario, along with a dismal report card on America's infrastructure from the ASCE (American Society of Civil Engineers).
While we can't predict what the next big disaster will be, or where it will strike, we do know that whatever comes over the next year or two will be greatly complicated by our ongoing pandemic, and global recession.And of course, to these catastrophic disasters we can always add floods, droughts, heatwaves, blizzards, and other weather related events both in the United States, and around the world, which could affect food harvests, supply chains, and global stability.
As the (above) graphic illustrates (see #NatlPrep: FEMA National Household Preparedness Survey), while we've seen some improvement over past few years, Americans still have a long way to go if we are to cultivate a culture of preparedness.
The goal is to have every American household prepared to handle at least a week without essential services (electricity, running water, open grocery stores, etc.) in the event of a local or regional disaster. And frankly, 2 weeks would be better.
In recent years preparedness has gotten a bit of a bad name. The popular image of a prepper - promulgated by the media and cable TV - is that of a nut out gathering squirrels, as they wait anxiously for doomsday.
While that archetype undoubtedly exists, most `preppers' are regular folks who gear up to deal with more reasonable, and more survivable, scenarios like hurricanes, floods, blizzards, and yes, even pandemics.
While I don't consider myself a survivalist (I don't own a stitch of camo), my years as a paramedic, and decades living on sailboats and in the backwoods of Missouri, have instilled in me a strong desire to be prepared for emergencies.
I know first hand what it is like when things go pear-shaped, and there's no one to call for help.
Which is why I promote the idea of having, and being, a `disaster buddy',and why when I give presents to friends and family, they are almost always in the form of `preps' (see The Gift Of Preparedness - 2019 Holiday Edition).
Because, no matter what the emergency, the advantage always goes to those who are best prepared.I hope you'll join me during the month of September in improving your, and your family's, resilience against the unexpected. Even little preps - like having a week's worth of food and water in the pantry - can pay big dividends in a disaster.