#18,807
Although H5N1 has a fearsome reputation, and has been credited with causing 985 confirmed human infections and 473 deaths (48% CFR), we've long known that some variants of HPAI H5N1 have been more pathogenic in humans than others.
As the modified WHO chart above illustrates, the oft-cited 50% CFR (Case Fatality Rate) of HPAI H5N1 was only true in a handful of - mostly Asian - nations, and since 2020 has averaged 14% (18 of 124 cases).
This abrupt drop in H5N1 severity hasn't been across the board, however, since Cambodia has reported 29 cases over the past 30 months, and at least 12 deaths (41%).
Even in the United States, where 71 cases (and 1 fatality) have been confirmed, we've seen a marked difference in the severity of human infection between the bovine B3.13 strain, and the D1.x strain of the virus.
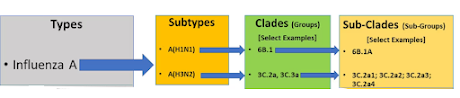
As we've discussed often, H5N1 is not a single virus - but rather an placeholder for a large (and growing) array of related clades, subclades, and genotypes which have emerged over the past 3 decades, and have either died off or continue to circulate around the globe.
Although the exact reasons are not known, given the tremendous diversity among H5N1 viruses, it is not surprising that some variants appear to be more pathogenic in humans (and other species) than others.
We've looked at a number of studies which have attempted to link past exposure to the post-2009 H1N1 seasonal flu virus to some (likely minor) degree of immunity to the Bovine B3.13 genotype of H5N1.
Two EID Journal Articles On Prior Immunity From A(H1N1)pdm09 Infection Against H5N1 (in Ferrets)
Preprint: Population Immunity to HPAI 2.3.4.4b A(H5N1) Viruses in the United States and the Impact of Seasonal Influenza on A(H5N1) Immunity
Preprint: Detection of Low Pre-existing Humoral Immunity Against Influenza Virus H5N1 clade 2.3.4.4b in Unexposed Individuals
This is a fascinating study, but due to its length and copyright issues, you'll need to read it on the journal's website. I've provided the link below.
Katherine H. Restori, Veronika Weaver, Devanshi R. Patel, Grace A. Merrbach, Kayla M. Septer , Cassandra J. Field , Michael J. Bernabe , Ethan M. Kronthal, Allen Minns , [...] , and Troy C. Sutton
23 Jul 2025 Vol 17, Issue 808
DOI: 10.1126/scitranslmed.adw4856
Excerpt from the press release from Penn State University follow.
Seasonal flu immunity protects against severe illness from bird flu in ferrets
A study in ferrets — which have remarkably similar respiratory systems to humans — suggests that widespread immunity to H1N1 seasonal influenza virus may explain why exposure to H5N1 bird flu causes only mild symptoms in humans
July 23, 2025
By Sara LaJeunesse
UNIVERSITY PARK, Pa. — The fatality rate for H5N1 highly pathogenic avian influenza in humans historically has been high, with more than half of people dying.
Why, then, is the current H5N1 bird flu outbreak — which has caused massive die-offs in wild birds, farmed poultry and even wild mammals — causing mostly mild symptoms in the people it has infected? New research, led by scientists at Penn State and the University of Pittsburgh and published today (July 23) in the journal Science Translational Medicine, indicates that immunity to a seasonal influenza virus known as pandemic H1N1 that began circulating in 2009, provides protection from severe illness from H5N1 in a laboratory animal model.
(SNIP)
To conduct their study, Sutton and his colleagues, including Valerie LeSage, a research assistant professor at the University of Pittsburgh who co-led the research, studied ferrets with immunity to three common types of seasonal flu: Influenza B, H1N1 and H3N2. They also studied a control group of ferrets that had no immunity to flu. Ninety days after infecting the ferrets with these common seasonal flu viruses, the team confirmed immunity by testing the animals’ blood for antibodies. Next, the team exposed the ferrets through an inoculation in the nose to a version of the H5N1 virus that caused an outbreak on mink farms in Spain in 2022.
They found that all the ferrets without immunity to the seasonal flu viruses, as well as those with immunity to Influenza B, became sick, lost weight and reached a humane endpoint. The H3N2-immune ferrets lost 10% of their body weight but all survived. In contrast, the ferrets with immunity to H1N1 did not lose any weight and all survived.
Next, the team studied the potential protective effects of the same three seasonal influenza viruses against the more recent H5N1 virus that has been circulating in dairy cattle. This time, instead of inoculating the ferrets with H5N1 in the nose, the team exposed ferrets with immunity to H1N1, H3N2 or without immunity to a seasonal virus, to ferrets already infected with an H5N1 virus from dairy cows. Sutton said by examining exposure to H5N1-infected ferrets, the team could assess the transmissibility of the virus in addition to the effects of pre-existing immunity.
The researchers found that upon exposure to ferrets with dairy cow H5N1 infections, ferrets without any influenza immunity rapidly developed severe and lethal disease. When exposed to H5N1-infected ferrets, all the ferrets with pre-existing immunity to H3N2 became infected and replicating H5N1 virus was detected in their noses. These ferrets lost weight and half of them reached a humane endpoint.
In contrast, only half of the ferrets previously infected with the 2009 H1N1 virus became infected, and the infected animals were protected against disease and had very low levels of viral replication in the nose.
“These findings demonstrate that pre-existing immunity to the 2009 H1N1 virus or H3N2 virus reduces the severity of H5N1 disease, with H1N1 providing even greater protection than H3N2,” Sutton said. “This study provides a potential explanation for the mostly mild disease we are seeing in humans, as humans already have immunity to H1N1.”
However, Sutton noted, as the H5N1 virus continues to circulate in animals, it has opportunities to evolve to become more dangerous.
- First, that ferrets are a good - but hardly perfect - analog for the pathogenicity of influenza A in humans.
- Second, the pre-immune ferrets (exposed to 2009 H1N1 & H3N2) used in this study do not share the same extended and messy flu exposure history as do most humans (see PLoS Path.: Childhood Immune Imprinting to Influenza A).
- Third, the bovine B3.13 genotype is but one of hundreds of HPAI H5N1 variants already in the wild, and there are no guarantees that it will emerge as the next pandemic contender.
- Fourth, we continue to watch other HPAI H5 subtypes - including H5N5 and H5N6 - which may someday supplant H5N1 as the dominant subtype. These are particularly worrisome because of their novel NA genes.
Hopefully, H5Nx encounters an insurmountable species barrier, and is never able to produce a pandemic (see Are Influenza Pandemic Viruses Members Of An Exclusive Club?).
But another pandemic - whether from influenza A, another coronavirus, or something out of left field - is inevitable. It's only a matter of time.