Credit Wikipedia
# 8852
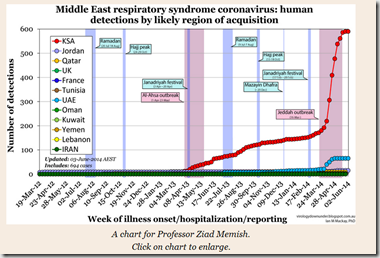
While MERS cases have thankfully declined over the summer months, there remain concerns that it may return this fall during the time of the Hajj (early October), when roughly 2 million devout from around the world will make the pilgrimage to the Saudi Holy sites.
Mass gatherings such as the Hajj, Chunyun (Chinese New Years-Spring Festival), Carnival in Rio, Mardi Gras, and the Super Bowl all bring together huge groups of people, and all have the potential to amplify the transmission of diseases.
The good news is, that while mass gatherings may provide greater opportunities for disease outbreaks, history has shown that major epidemic outbreaks have been rare. One notable exception was the 1918 Liberty Loan Parade in Philadelphia, which was attended by as many as 200,000 people.
During the 1918 Pandemic, most cities instituted strict public health ordinances; they closed schools, movie houses, pool rooms, restaurants . . even churches. But Philadelphia went ahead with a massive parade on September 28th of that year, apparently heartened by the low number of flu cases reported in Pennsylvania to that point.
Over the next three weeks, at least 6,081 deaths from influenza and 2,651 deaths from pneumonia were registered in Pennsylvania, most occurring in Philadelphia (CDC source).
While a particularly dramatic example, concerns over seeing a repeat of this sort of thing run high enough that mass gathering medicine has now become a specialty (see Lancet: Mass Gathering and Health), and public health agencies around the world gear up for every large gathering event (see How The ECDC Will Spend Your Summer Vacation & The ECDC Risk Assessment On Brazil’s FIFA World Cup)
Although they carry the highest potential impact, public health concerns for these mass gathering events go far beyond exotic diseases like MERS and pandemic influenza.
Tuberculosis, pneumococcal disease, meningococcal disease, chickenpox, pertussis, polio, cholera, mumps and a plethora of other respiratory viral and bacterial diseases all rank high on the list of potential infectious disease threats, along with concerns over food-borne and vector borne illnesses.
To try to quantify the risks of acquiring, and spreading, some of the more commonly seen respiratory pathogens during the Hajj, a group of researchers have – for the second year in a row – tested a group of Hajjis both before and after the Hajj for carriage of a variety of bacterial and viral pathogens.
While carriage these pathogens among test subjects was high prior to attending the Hajj, they increased markedly immediately post-Hajj, indicating efficient transmission of several respiratory pathogens.
Samir Benkouiten, Rémi Charrel, Khadidja Belhouchat, Tassadit Drali, Antoine Nougairede, Nicolas Salez, Ziad A. Memish, Malak al Masri, Pierre-Edouard Fournier, Didier Raoult, Philippe Brouqui, Philippe Parola, and Philippe Gautret
Abstract
Pilgrims returning from the Hajj might contribute to international spreading of respiratory pathogens. Nasal and throat swab specimens were obtained from 129 pilgrims in 2013 before they departed from France and before they left Saudi Arabia, and tested by PCR for respiratory viruses and bacteria. Overall, 21.5% and 38.8% of pre-Hajj and post-Hajj specimens, respectively, were positive for ≥1 virus (p = 0.003). One third (29.8%) of the participants acquired ≥1 virus, particularly rhinovirus (14.0%), coronavirus E229 (12.4%), and influenza A(H3N2) virus (6.2%) while in Saudi Arabia. None of the participants were positive for the Middle East respiratory syndrome coronavirus. In addition, 50.0% and 62.0% of pre-Hajj and post-Hajj specimens, respectively, were positive for Streptococcus pneumoniae (p = 0.053). One third (36.3%) of the participants had acquired S. pneumoniae during their stay. Our results confirm high acquisition rates of rhinovirus and S. pneumoniae in pilgrims and highlight the acquisition of coronavirus E229.
More than 2 million Muslims gather annually in Saudi Arabia for a pilgrimage to the holy places of Islam known as the Hajj. The Hajj presents major public health and infection control challenges. Inevitable overcrowding within a confined area with persons from >180 countries in close contact with others, particularly during the circumambulation of the Kaaba (Tawaf) inside the Grand Mosque in Mecca, leads to a high risk pilgrims to acquire and spread infectious diseases during their time in Saudi Arabia (1), particularly respiratory diseases (2). Respiratory diseases are a major cause of consultation in primary health care facilities in Mina, Saudi Arabia, during the Hajj (3). Pneumonia is a leading cause of hospitalization in intensive care units (4).
<SNIP>
In this study, we confirmed that performing the Hajj pilgrimage is associated with an increased occurrence of respiratory symptoms in most pilgrims; 8 of 10 pilgrims showed nasal or throat acquisition of respiratory pathogens. This acquisition may have resulted from human-to-human transmission through close contact within the group of French pilgrims because many of them were already infected with HRV or S. pneumoniae before departing from France. Alternatively, the French pilgrims may have acquired these respiratory pathogens from other pilgrims, given the extremely high crowding density to which persons from many parts of the world are exposed when performing Hajj rituals. Finally, contamination originating from an environmental source might have played a role.
(Continue . . . )
If all of this sounds vaguely familiar, you may recall the following Clinical Infectious Diseases study (also co-authored by Ziad Memish) - Unmasking Masks in Makkah: Preventing Influenza at Hajj – from 2012
.
Each year more than 2 million people from all over the world attend the Hajj pilgrimage to Saudi Arabia. At least 60% of them develop respiratory symptoms there or during outward or homebound transit [1, 2] During recent interpandemic years, approximately 1 in 10 pilgrims with respiratory symptoms in Makkah have had influenza detected by polymerase chain reaction tests of respiratory samples [3, 4]. Pneumonia is the leading cause of hospitalization at Hajj, accounting for approximately 20% of diagnoses on admission [5].
All of this has the potential to help seed emerging strains of viral and bacterial diseases around the world, and while perhaps not nearly as dramatic as a pandemic outbreak, still carries with it considerable public health implications.
But this year – with fears that MERS might spread internationally – public health officials must also be concerned with those 60%-80% of Hajjis who will return home this fall with respiratory symptoms.
We’ve discussed the The Limitations Of Airport Screening in the past, so in a different approach, the following sign appears in airports in the United Kingdom urging self-reporting of illness and travel history to one’s doctor. Similar signs have been erected at airports around the globe (see MERS Advisories Go Up In Some US Airports).
.

While we don’t know if MERS will make a return during the Hajj, given the high incidence of respiratory illnesses reported in returning Hajjis, I expect that we’ll be hearing a lot about testing for suspected MERS-CoV this fall.
Undoubtedly the vast majority of these travelers will have influenza, Rhinoviruses, RSV, HCoV E229, or simple bacterial pneumonia, but ruling out the MERS coronavirus is going to represent a major public health logistical challenge, even in places like the UK and the United States.
How well this can be accomplished in low-resource regions of the world, to where many of the pilgrims will be returning, remains to be seen. The hope is that the level of MERS cases will remain low in the Middle East during the time of the Hajj, as it has for the past two years.
Stay tuned.