#17,666
Highly Pathogenic Avian Influenza (HPAI) H5N1 was first detected in Chinese poultry 27 years ago (see WHO timeline below), jumped to humans for the first time a year later (1997), and then - following a massive culling of Hong Kong's poultry - seemingly went to ground for more than 5 years.
H5N1's return in 2003 - first reported in Hong Kong, followed by South Korea and then Thailand - sent shock waves through the influenza research community, but was largely overshadowed by the global spread of SARS-COV, which had begun in China in 2002 (see SARS and Remembrance).
In January of 2004 H5N1 turned up in Vietnam and Thailand - and now that countries knew what to look for - reports of human cases (and deaths) began to mount. Reports of wild birds dying from the virus began to emerge, along with reports of infections and deaths among tigers and lions in Southeast Asia zoos.
For those first few years, H5N1 remained primarily an Asian problem, infecting poultry, and spreading - by human activity and wild birds - relatively slowly. But the virus was also evolving, and honing its ability to spread.
During the great H5N1 diaspora of 2006, we saw highly pathogenic H5N1 go from being a geographically limited threat to a global problem when, in a little over a year’s time, it spread from 15 southeast Asian nations to much of Western Europe and into parts of west Africa.
By the end of 2007, more than 60 nations had reported this avian flu virus either in poultry or wild birds.
H5N1 wasn't the only avian flu virus we were tracking - other `minor' players included LPAI H5N2, HPAI H7Nx, and LPAI H9N2 - but H5N1 was the deadliest, and most concerning novel flu virus on our radar.
But for reasons not well understood, after 2007 H5N1 halted its global expansion. H5N1 activity actually began to decline in 2008, and while it remained endemic in a handful of countries like Vietnam, Bangladesh, India, Indonesia, Egypt, and China, its global retreat was dramatic.
By 2012, the number of countries reporting HPAI had dropped from 60 to 15, and many were predicting the H5N1 threat would soon be over.
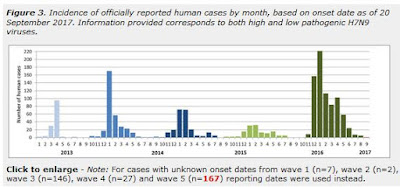
In 2013, everything changed; H7N9 emerged in China, and launched its first (of 5) seasonal epidemics, killing hundreds (see China’s MOA: H7N9 Fatalities Higher Than Previously Announced).
Over the next 12 months we'd see scattered H10N8 infections reported in China, a new, and highly virulent (in poultry) HPAI H5N8 virus (clade 2.2.4.4) arrive in South Korea from China. We also saw new HPAI H5N6 virus emerge in China, which began spilling over into humans in the spring of 2014.
At the same time, the H5N1 virus continued to reinvent itself - notably into clade 2.3.2 in 2009 (see 2011 EID Journal New Avian Influenza Virus (H5N1) in Wild Birds, Qinghai, China), and clade 2.3.2.1c in 2015 (see Novel H5N1 Reassortment Detected In Migratory Birds - China).
While H5N1 retreated again, H5N8 clade 2.3.4.4 (followed by reassorted H5N6 and H5N1 variations) took the lead, sparking Europe's first major avian epizootic in 2016. That lineage continued to evolve, and has - since 2021 - spread globally.
But it is not alone. We've also seen the spillover of other avian viruses to humans, including H3N8, H5N6, H10N3, and H9N2, and the emergence of many other concerning subtypes in poultry, and wild birds, around the world.
Influenza's superpower is its ability to share genetic material - via reassortment - and reinvent itself.
As one might expect, the more subtypes in circulation, the greater the opportunities there are for new subtypes to emerge. Like a snowball rolling down a hill, avian influenza continues to pick up both mass and speed.
All of which brings us to a review article, penned by scientists at the CDC, which examines the rapid spread and diversification of avian influenza viruses since 2013. They also highlight - as has been often discussed in this blog - the regrettable gaps in surveillance and reporting around the world on these, and other, zoonotic threats.
I've only reproduced the abstract. This is quite a detailed report so many will want to follow the link to read it in its entirety. The CDC published as summary HERE.
Authors of this article:Christine M Szablewski 1 ; Chelsea Iwamoto 1 ; Sonja J Olsen 1 ; Carolyn M Greene 1 ; Lindsey M Duca 1 C Todd Davis 1 Kira C Coggeshall 2 ; William W Davis 1 ; Gideon O Emukule 1 ; Philip L Gould 1 ; Alicia M Fry 1 ; David E Wentworth 1 ; Vivien G Dugan 1 ; James C Kile 1 ; Eduardo Azziz-Baumgartner 1
Abstract
Background:
Avian influenza (AI) virus detections occurred frequently in 2022 and continue to pose a health, economic, and food security risk. The most recent global analysis of official reports of animal outbreaks and human infections with all reportable AI viruses was published almost a decade ago. Increased or renewed reports of AI viruses, especially high pathogenicity H5N8 and H5N1 in birds and H5N1, H5N8, and H5N6 in humans globally, have established the need for a comprehensive review of current global AI virus surveillance data to assess the pandemic risk of AI viruses.
Objective:
This study aims to provide an analysis of global AI animal outbreak and human case surveillance information from the last decade by describing the circulating virus subtypes, regions and temporal trends in reporting, and country characteristics associated with AI virus outbreak reporting in animals; surveillance and reporting gaps for animals and humans are identified.
Methods:
We analyzed AI virus infection reports among animals and humans submitted to animal and public health authorities from January 2013 to June 2022 and compared them with reports from January 2005 to December 2012. A multivariable regression analysis was used to evaluate associations between variables of interest and reported AI virus animal outbreaks.
Results:
From 2013 to 2022, 52.2% (95/182) of World Organisation for Animal Health (WOAH) Member Countries identified 34 AI virus subtypes during 21,249 outbreaks. The most frequently reported subtypes were high pathogenicity AI H5N1 (10,079/21,249, 47.43%) and H5N8 (6722/21,249, 31.63%). A total of 10 high pathogenicity AI and 6 low pathogenicity AI virus subtypes were reported to the WOAH for the first time during 2013-2022. AI outbreaks in animals occurred in 26 more Member Countries than reported in the previous 8 years.
Decreasing World Bank income classification was significantly associated with decreases in reported AI outbreaks (P<.001-.02). Between January 2013 and June 2022, 17/194 (8.8%) World Health Organization (WHO) Member States reported 2000 human AI virus infections of 10 virus subtypes. H7N9 (1568/2000, 78.40%) and H5N1 (254/2000, 12.70%) viruses accounted for the most human infections. As many as 8 of these 17 Member States did not report a human case prior to 2013.
Of 1953 human cases with available information, 74.81% (n=1461) had a known animal exposure before onset of illness. The median time from illness onset to the notification posted on the WHO event information site was 15 days (IQR 9-30 days; mean 24 days). Seasonality patterns of animal outbreaks and human infections with AI viruses were very similar, occurred year-round, and peaked during November through May.
Conclusions:
Our analysis suggests that AI outbreaks are more frequently reported and geographically widespread than in the past. Global surveillance gaps include inconsistent reporting from all regions and human infection reporting delays. Continued monitoring for AI virus outbreaks in animals and human infections with AI viruses is crucial for pandemic preparedness.
JMIR Public Health Surveill 2023;9:e46383
doi:10.2196/46383