#17,823
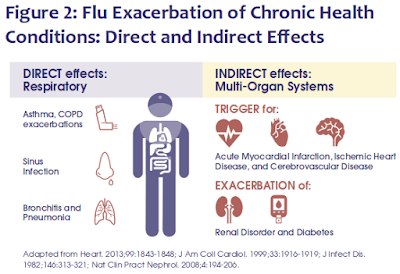
Although we've discussed the long term impacts of seasonal influenza many times over the years (see here, here, and here), most people today still regard non-pandemic flu as a short-term, acute infection, that is only really dangerous for the elderly or those with serious comorbidities.
Given the frequency of flu infections we experience over a lifetime, it's a comforting - if not entirely accurate - perception.
While we hear a lot about `Long COVID' these days, prior to the COVID pandemic there were estimated to be as many as 2.5 million Americans suffering (mostly in silence) from Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Although the exact cause of ME/CFS remains unknown, many doctors believe it can be triggered by a viral illness (see The viral origin of myalgic encephalomyelitis/chronic fatigue syndrome).
Dozens of studies over the past 3 years have shown that a significant percentage of COVID survivors are left with long-lasting, sometimes chronic, health problems; syndromes that often look remarkably like ME/CFS.
A few of those studies include:
Study: SARS-CoV-2 Infection and Viral Fusogens Cause Neuronal and Glial Fusion that Compromises Neuronal Activity
JAMA: Additional Evidence Of A Post-COVID/Diabetes Link
Nature: Long-term Cardiovascular Outcomes of COVID-19
The Lancet: Neurological and Psychiatric Risk Trajectories After SARS-CoV-2 Infection
MMWR: Post–COVID-19 Symptoms and Conditions Among Children and Adolescents
In the decade following the last great influenza pandemic (1918) the world saw another mysterious epidemic of neurological diseases called Encephalitis Lethargica (EL). It has been estimated that between 1 and 5 million people were afflicted with EL between 1917 and 1927.
Roughly 1/3rd died during the acute phase of the illness - while many of the survivors would go on to develop Parkinsonian features and other profound neurological sequelae, often years later.
Originally thought to be a sequelae of the pandemic H1N1 virus, more recently a 2012 study presented a case for the EL epidemic having been caused by an enterovirus (see Evidence for an enterovirus as the cause of encephalitis lethargica).
Throughout history, there have been reports of similar strange outbreaks following large epidemics, including febris comatosa which sparked a severe epidemic in London between 1673 and 1675, and in 1890 in Italy, in the wake of the 1889–1890 influenza pandemic, a severe wave of somnolent illnesses (nicknamed the "Nona") appeared.It now appears likely that many viral infections can leave behind a `post-viral' syndrome in some percentage of cases.
While falling short of proving causation, it adds to the preponderance of evidence.
A month later (Feb 2023) we looked at NIH Preprint: Comparing The Impact Of `Long Flu' to `Long COVID', which found a similar - but less severe - post-viral syndrome in those who recovered from seasonal influenza.
All of which brings us to a study, published in The Lancet, which compares the incidence and severity `Long-Flu' to `Long-COVID' from health-care databases of the US Department of Veterans Affairs.
While the post-COVID syndrome was deemed more severe, post-influenza sequelae was significant, and sometimes life threatening.
First a link and some excerpts from a news release from the Washington School of Medicine in St. Louis, followed by a link and a short excerpt from the study. You'll want to follow the links to read both in their entirety.
I'll have a brief postscript after the break.
NEWS RELEASE
‘Long flu’ has emerged as a consequence similar to long COVID
Study shows patients hospitalized for flu or COVID-19 face increased risk of long-term health problems, death
by Kristina Sauerwein•December 14, 2023
New research from Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care System comparing the viruses that cause the flu and COVID-19 shows that people hospitalized with seasonal influenza also can suffer long-term, negative health effects, especially involving their lungs and airways. The study also found that in the 18 months after infection, patients hospitalized for either COVID-19 or seasonal influenza faced an increased risk of death, hospital readmission, and other health problems.
Since the COVID-19 pandemic began, extensive research has emerged detailing the virus’s ability to attack multiple organ systems, potentially resulting in a set of enduring and often disabling health problems known as long COVID. Now, new research from Washington University School of Medicine in St. Louis and the Veterans Affairs St. Louis Health Care System indicates that people hospitalized with seasonal influenza also can suffer long-term, negative health effects, especially involving their lungs and airways.
The new study comparing the viruses that cause COVID-19 and the flu also revealed that in the 18 months after infection, patients hospitalized for either COVID-19 or seasonal influenza faced an increased risk of death, hospital readmission, and health problems in many organ systems. Further, the time of highest risk was 30 days or later after initial infection.
“The study illustrates the high toll of death and loss of health following hospitalization with either COVID-19 or seasonal influenza,” said senior author Ziyad Al-Aly, MD, a clinical epidemiologist at Washington University. “It’s critical to note that the health risks were higher after the first 30 days of infection. Many people think they’re over COVID-19 or the flu after being discharged from the hospital. That may be true for some people. But our research shows that both viruses can cause long-haul illness.”
The findings are published Dec. 14 in The Lancet Infectious Diseases.
Long-term outcomes following hospital admission for COVID-19 versus seasonal influenza: a cohort study
Yan Xie, PhD Taeyoung Choi, MS Ziyad Al-Aly, MD
Published: December 14, 2023 DOI:https://doi.org/10.1016/S1473-3099(23)00684-9
Interpretation
Although rates of death and adverse health outcomes following hospital admission for either seasonal influenza or COVID-19 are high, this comparative analysis shows that hospital admission for COVID-19 was associated with higher long-term risks of death and adverse health outcomes in nearly every organ system (except for the pulmonary system) and significant cumulative excess DALYs than hospital admission for seasonal influenza. The substantial cumulative burden of health loss in both groups calls for greater prevention of hospital admission for these two viruses and for greater attention to the care needs of people with long-term health effects due to either seasonal influenza or SARS-CoV-2 infection.
Just over two years ago we learned that repeated COVID infections increase the risks for developing chronic health problems (see Nature: Acute and Postacute Sequelae Associated with SARS-CoV-2 Reinfection), and it is entirely possible (perhaps even likely) the same holds true for other viral infections.
Despite this growing evidence, society has decided to trivialize the impact of COVID infection, much in the same way it has trivialized the flu for decades.
Uptake of the COVID and Flu vaccine - are down, and you rarely see anyone wearing a mask in public, or staying home with the sniffles or a cough. Instead, we act as if these viruses were benign.
While most people will recover from COVID or flu infection without long-term damage, some percentage won't be as lucky. And that not only presents individual health challenges, but societal challenges as well.
All of which makes COVID, influenza, and a plethora of other respiratory viruses well worth avoiding if at all possible.