Credit CDC
# 9626
In China, it is often called Chunyun, Chinese New Year, or simply, The Spring Festival. In Korea it is called Seollal. While in Vietnam it is celebrated as Tết Nguyên Đán ; the Feast of the First Morning. Tết for short.
By whatever name, the Lunar New Year is undoubtedly the most important holiday in all of Asia
Each year it inspires the largest migration of humans on the planet as hundreds of millions flee the big cities and return to their home towns for a few days to attend a reunion dinner with their families - preferably on the eve of the lunar New Year.
The entire Spring festival travel season begins about 2 weeks before the Lunar New Year, and runs for about 6 weeks. With the New Year falling on February 19th this year, we are 10 days from the start of an event which could see more than 3 billion passenger journeys – mostly by crowded train – across Asia over the next 60 days.
Ducks, geese, and chickens figure prominently at many of these family dinners, and the live markets do tremendous business during this time of year. Many cities are therefore reluctant to halt the trade in live birds until after the New Year.
As all of this occurs during the height of the regular flu season, and concurrent with China’s winter spike in avian flu cases, public health agencies are understandably alert to the possibility of seeing a post-holiday surge in illnesses, including influenza, measles, malaria, tuberculosis and food poisoning.
In 2010, in The Impact Of Mass Gatherings & Travel On Flu Epidemics , we looked at a study published in BMC Public Health, that looked at and attempted to quantify the impacts of mass gatherings and holiday travel on the spread of an influenza epidemic.
And in 2011, in Viruses With A Ticket To Ride, we looked at research that appeared in BMC Infectious Diseases, that looked at the incidence of ARI (Acute Respiratory Infection) presenting within 5 days of train or tram travel in the UK. They found that recent bus or tram use within five days of symptom onset was associated with an almost six-fold increased risk of consulting for ARI.
While seemingly a strong finding, this observational study was limited by its small size, the fact that it was only conducted in a single location (Nottingham, UK), and that it was conducted during a normal flu season, not a pandemic.
The good news is, that while mass gatherings may provide greater opportunities for disease outbreaks, history has shown that major epidemic outbreaks have been a rarity (for a notable exception, see The Impact Of Mass Gatherings & Travel On Flu Epidemics).
While the risks of seeing a major disease outbreak in any given year are small, public health authorities must anticipate and prepare for the worst. A few days ago Taiwan’s CDC issued the following advisory for those intending to travel to mainland China.
Press Releases
( 2015-01-22 )
As the ongoing H7N9 outbreak in China escalates and the winter break and the Chinese New Year Holiday are fast approaching, the Taiwan Centers for Disease Control (Taiwan CDC) reminds travelers visiting China to heighten their vigilance for avian influenza and practice good personal hygiene and avoid contact with poultry and birds and consume only thoroughly cooked poultry and eggs in order to ward off infection.
In light of a significant increase in the number of H7N9 cases (29), which were confirmed in mostly Fujian Province and Guangdong Province, China, last week, Taiwan CDC has issued a travel notice of Level 2: Alert for avian influenza to Xinjiang Uyghur Autonomous Region, Jiangsu Province, Zhejiang Province, Guangdong Province, Fujian Province, Shanghai City, and Jiangxi Province, and a travel notice of Level 1: Watch for avian influenza to the other provinces and cities in China, excluding Hong Kong and Macau.
<SNIP>
Taiwan CDC once again urges travelers visiting China to practice good personal hygiene such as washing hands frequently and putting on a mask when coughing and take preventive measures such as avoiding direct contact with poultry and birds or their droppings/dead bodies, and consuming only thoroughly cooked poultry and eggs. If influenza-like illness symptoms develop upon arriving in Taiwan, please voluntarily notify the airline crew and the quarantine officer at the quarantine station in the airport. If symptoms such as fever and cough develop after returning to Taiwan, please put on a surgical mask and seek immediate medical attention. Moreover, please inform the physician of the recent travel and exposure history to facilitate diagnosis and treatment. For more information, please visit the Taiwan CDC website at http://www.cdc.gov.tw or call the toll-free Communicable Disease Reporting and Consultation Hotline, 1922 (or 0800-001922).
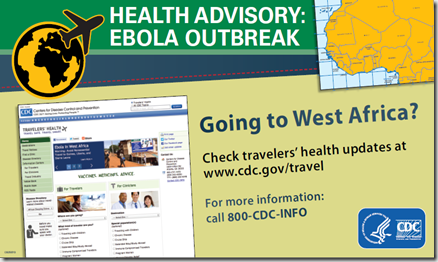
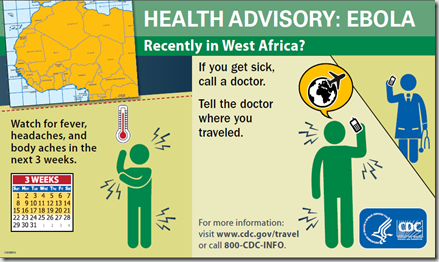
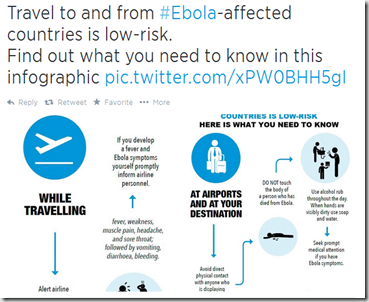
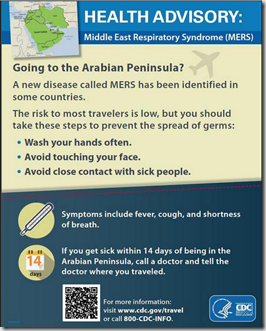
And for some health and safety tips from America’s CDC, we have following from the CDC Travelers Health Website.
Released: January 13, 2015
The Year of the Goat begins on February 19, 2015, and many travelers will visit Asia to celebrate the Lunar New Year. If you are traveling to Asia, plan ahead for a safe and healthy trip.
Every destination has unique health issues of which travelers need to be aware. To find specific information about the places you are traveling, visit our destination pages. In addition to being up-to-date on routine vaccines, you will find vaccine and medicine recommendations, along with many other tips for safe and healthy travel.
What can travelers do to protect themselves?
Before your trip:
- Schedule an appointment with your healthcare provider at least 4–6 weeks before you depart. Talk to your doctor or nurse about vaccines and medicines recommended for your destination. Travelers who want to reduce their risk of seasonal flu should receive the flu vaccine at least 2 weeks before departure. See the Travel Clinics webpage for help in finding a travel medicine clinic near you.
- Consider travel health and medical evacuation insurance.
- Pack a travel health kit.
During your trip:
- Choose safe transportation: Motor vehicle crashes are the #1 killer of healthy US citizens in foreign countries. Read about ways to prevent transportation injuries by visiting the Road Safety page.
- Reduce your exposure to germs: Wash your hands often, and avoid contact with people who are sick. Read more about reducing your exposure to germs in the “Stay Healthy and Safe” section of the destination page.
- Prevent mosquito bites: Diseases spread by mosquitoes, such as malaria, dengue, chikungunya, and Japanese encephalitis, are common throughout Asia. Read more about ways to prevent bug bites by visiting the Avoid Bug Bites page. You may also need to take prescription medicine to protect against malaria or get a vaccine against Japanese encephalitis. Talk to your doctor or nurse about prevention steps that are right for you and your destination.
- Follow food and water safety guidelines: Eating contaminated food and drinking contaminated water can cause illnesses such as hepatitis A, typhoid fever, and travelers’ diarrhea. Read about how to prevent these diseases by visiting the Safe Food and Water page on the Travelers’ Health website.
- Do not touch birds, pigs, or other animals, and avoid farms and poultry markets: Bird flu strains, such as H7N9 and H5N1, are flu viruses that have been seen in China.
- If you feel sick during your trip:
- Talk to a doctor or nurse if you feel seriously ill, especially if you have a fever.
- For more information about medical care abroad, see Getting Health Care Abroad.
- Avoid contact with other people while you are sick.
After your trip:
- If you are not feeling well after your trip, you may need to see a doctor. If you need help finding a travel medicine specialist, see Find a Clinic. Be sure to tell your doctor about your travel, including where you went and what you did on your trip. Also tell your doctor if you were bitten or scratched by an animal while traveling.
- If your doctor prescribed antimalarial medicine for your trip, keep taking the rest of your pills after you return home. If you stop taking your medicine too soon, you could still get sick.
- Malaria is always a serious disease and may be deadly. If you become ill with a fever either while traveling in a malaria risk area or for up to 1 year after you return home, you should seek immediate medical attention and should tell the doctor about your travel history.
- For more information, see Getting Sick after Travel.
While each year public health agencies gear up for the Hajj, The Lunar New Year, the Super Bowl, and other mass gathering events - and rarely does anything really bad happen - the old adage is true.
`When public health works, nothing happens’.