#17,043
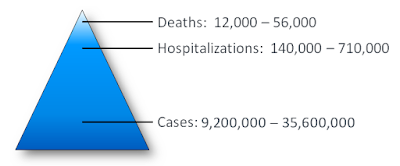
In a normal, non-pandemic year, seasonal flu kills roughly as many Americans as does gun violence, or car accidents. In a bad year - such as we saw in 2017-2018, influenza can kill as many as both of those combined.
But I digress.
This fall and winter, if the recent flu season in Australia - and summer outbreaks in China and Vietnam - are any gauge, we may see a much more robust flu/COVID season. But flu seasons are highly unpredictable, and can change course abruptly.
Yesterday the CDC released a (belated) preliminary assessment of the 2021-2022 flu season, one that while mild, extended unusually well into the summer months. As we've discussed often (see Why Flu Fatality Numbers Are So Hard To Determine), the CDC can only make educated estimates on the burden of influenza.
But based on their analysis, the CDC estimates seasonal influenza over the 2021-2022 season caused 9 million illnesses, 4 million medical visits, 100,000 hospitalizations, and 5,000 deaths.
Some excerpts from the CDC's analysis follows (note: the 10K hospitalizations in the conclusion is a typo, and should read 100K). I'll return with a bit more after the break.
The overall burden of influenza (flu) for the 2021-2022 season was an estimated 9 million flu illnesses, 4 million flu-related medical visits, 100,000 flu-related hospitalizations, and 5,000 flu deaths (Table 1).
For the past several years, CDC has used a mathematical model to estimate the numbers of influenza illnesses, medical visits, hospitalizations, and deaths (1-4). The methods used to calculate the estimates have been described previously (1-2). CDC uses the estimates of the burden of flu in the population to inform policy and communications related to influenza prevention and control.2021–2022 Burden Estimates
Since the emergence of SARS-CoV-2, influenza activity has been lower than observed before the pandemic. Compared with influenza seasons prior to pandemic, the 2021–2022 influenza season was mild and occurred in two waves, with a higher number of hospitalizations in the second wave. Influenza activity in the United States during the 2021–2022 season began to increase in November, declined in January 2022, increased again in March 2022 and remained elevated until mid-June 2022. The season was characterized by two distinct waves and predominately influenza A virus circulation. Overall, influenza A(H3N2) viruses were the most commonly detected influenza viruses this season. The 2021-22 season is described as having low severity**; however, the effect of influenza differed by age group and the severity of the season in some age groups was higher– hospitalization rates among older adults aged ≥65 years old were higher compared with other age groups (5).
CDC estimates that the burden of illness during the 2021–2022 season was low with an estimated 9 million people sick with flu, 4 million visits to a health care provider for flu, 100,000 hospitalizations for flu, and 5,000 flu deaths (Table 1). The number of cases of influenza-associated illness, medically attended illnesses, hospitalizations, and deaths were the lowest since the 2011-2012 season which was the first full season following the influenza A(H1N1)pdm09 pandemic (6). Adoption of mitigation measures intended to prevent the spread of COVID-19 may have also impacted the timing or severity of influenza activity during the 2021-2022 season.
CDC’s estimates of hospitalizations and mortality associated with the 2021–2022 influenza season show that despite the co-circulation of SARS-CoV-2 and other respiratory viruses, influenza viruses do still cause severe disease and death. Older adults accounted for 83% of deaths, which is similar to recent seasons before the COVID-19 pandemic. These findings continue to highlight the fact that older adults are particularly vulnerable to severe disease with influenza virus infection and that influenza prevention measures such as vaccination are important to reducing the impact of the seasonal epidemics on the population and healthcare system.
Deaths in children with laboratory-confirmed influenza virus infection have been a reportable disease in the United States since 2004; 39 deaths were reported for the 2021-22 season as of September 24, 2022. Although it is possible that reported deaths may under-estimate the true number of deaths for this age group, no deaths in children (aged <18 years) were observed through the Influenza Hospital Surveillance Network (FluSurv-NET) during the 2021-2022 influenza season. As a result, it was not possible to estimate deaths in this age group.
Conclusion
During the 2021-2022 influenza season, CDC estimates that influenza was associated with 9 million illnesses, 4 million medical visits, 10,000 hospitalizations, and 5,000 deaths. The influenza burden was similar to the burden observed during the 2011-2012 season.
** Some parameters for evaluation influenza season severity were updated staring in 2021-22. More information is available.
Yesterday the CDC announced their 2022-2023 Flu Vaccination Campaign Kickoff amid concerns that fewer Americans will roll up their sleeves for the flu vaccine this fall. An NFID (National Foundation For Infectious Diseases) poll, released this week, suggest that only 49% of U.S. adults plan to get the flu shot this year.
Following a mild flu season in 2021-2022, NFID survey shows only 49% of US adults plan to get a flu vaccine this season
Contact: Diana Olson, dolson@nfid.org, 301-656-0003 x140
Bethesda, MD (October 4, 2022)—With a potentially severe respiratory season ahead, about half of all US adults remain vulnerable to influenza (flu), according to new data released today by the National Foundation for Infectious Diseases (NFID). The new NFID survey of US adults found that only 49% plan to get a flu vaccine during the 2022-2023 flu season. Leading health experts from NFID and the Centers for Disease Control and Prevention (CDC) are urging everyone age 6 months and older to get vaccinated against flu now, amid concerns of a potentially severe season in the US.
Despite these disincentives, I've already gotten my shot this year, and encourage others to do so as well.
First, a mild flu season last year doesn't guarantee a repeat this year, and no one is sure what a severe flu/COVID season will look like. Some studies suggest co-infection produces more severe illness, while others do not.
This year, we are also on heightened alert for human infection with novel swine variant and avian influenza viruses. While the seasonal flu shot isn't designed to protect against either of these novel viruses, bad things can happen when an individual is infected with a seasonal and novel virus at the same time.

A novel/seasonal flu reassortment is not a new concern, nor is this scenario limited to H5N1, or a swine variant virus. Anytime two different flu viruses inhabit the same host (human, avian, porcine, etc.) at the same time, the potential for seeing a reassortant virus exists (see MMWR: Seasonal H3N2 & H1N1pdm09 Reassortant Infection — Idaho, 2019).
Most reassortments end up as evolutionary failures, but every once in a while a genetic winner emerges. And given the events of the past couple of years, there is no sense aiding and abetting these viral contenders.
Admittedly, the seasonal flu shot isn't as effective as we'd like, but most years it provides moderate protection against infection, and for those over 65, there are more effective high-dose and adjuvanted vaccines available.
While the current flu vaccine is far from perfect, and can’t promise 100% protection, it – along with practicing good flu hygiene (washing hands, covering coughs and/or wearing a mask & staying home if sick) – remains your best strategy for avoiding the flu and staying healthy this winter.Even when the flu shot doesn't prevent infection, there is growing evidence it can reduce the severity of one's illness, and reduce your odds of having a heart attack or stroke (see Study Suggests Flu Vaccine May Lower Stroke Risk in Elderly ICU Patients).

