# 9499
Hong Kong’s Centre For health Protection (CHP) was formed in the wake of that city’s disastrous SARS epidemic a little over a decade ago. Since then the CHP has gained a reputation for openness, and mounting a rapid response to any disease threat.
Today they’ve released a detailed statement on their investigation into the first imported H7N9 case from the Chinese mainland this winter.
While human-to-human transmission of the H7N9 virus has only rarely been reported, the incubation period is thought to be up to 10 days, and so arrangement are being made for asymptomatic contacts to be quarantined at the Lady MacLehose Holiday Village in Sai Kung (description below).
Located within Sai Kung Country Parks at Pak Tam, Sai Kung, the Lady MacLehose Holiday Village has an air of tranquility and presents a charming view of the woody hillsides. Each bungalow, which can accommodate 3 to 15 persons, is self-contained with a sitting room, bedroom(s) and a toilet with shower facilities. The Camp has a capacity of 280 campers. Hirers please note that Camp facilities, such as bungalows, recreational facilities, canteen, etc., are located on different spots of a slope and connected by pavements.
We’ve seen similar arrangements in the past both in Hong Kong and in Singapore (see Singapore MOH Puts Quarantine Chalets On Standby). This is the 11th imported case of H7N9 in Hong Kong, and they are well practiced in the handling of such cases.
Update of human case of avian influenza A(H7N9)
The Department of Health (DH) today (December 28) reported the latest updates of the first confirmed human case of avian influenza A(H7N9) in Hong Kong this winter, and again urged the public to maintain strict personal, food and environmental hygiene both locally and during travel.
Epidemiological investigations and control measures
---------------------------------------------------
Epidemiological investigations by the Centre for Health Protection (CHP) of the DH so far located 12 close contacts and 47 other contacts of the patient.
(A) Close contactsThe close contacts have been put under quarantine and prescribed with antiviral presumptive treatment until the completion of the five-day treatment or ten days after last exposure to the patient, whichever is earlier. They include:
- Seven family members (revised from nine after further enquiries) in which one was symptomatic and tested negative for H7 virus while the rest being asymptomatic; and
- Five in-patients admitted to the same cubicle as the patient in Tuen Mun Hospital (TMH) in which one was symptomatic and tested negative for H7 virus while the rest being asymptomatic.
- Two travel collaterals are yet to be reached and follow-up is underway.
(B) Other contacts
The other contacts have been put under medical surveillance and they include:
- A total of 42 healthcare workers who took care of the patient in TMH in which two were symptomatic and tested negative for H7 virus while the rest being asymptomatic;
- Three asymptomatic ambulance officers involved in patient transfer; and
- Two asymptomatic visitors of the cubicle to which the patient was admitted.
The two private doctors whom the patient consulted are yet to be reached and follow-up is underway.
The CHP is communicating with the health authorities of Guangdong Province to follow up the situation during the patient's stay in the Mainland.As the patient did not visit any wet markets or contact live poultry in Hong Kong during the incubation period, based on information available thus far, it is classified as an imported case. Investigations are ongoing.
The Lady MacLehose Holiday Village in Sai Kung under the Leisure and Cultural Services Department is being converted as a quarantine centre. Asymptomatic close contacts will be quarantined there.
Upon activation of the Serious Response Level (SRL) under the Preparedness Plan for Influenza Pandemic last night (December 27), the DH immediately commenced enhanced surveillance, enhanced port health measures and risk communication accordingly.
Enhanced surveillance
---------------------
The CHP has enhanced surveillance of suspected cases in public and private hospitals, and will activate electronic reporting system to monitor cases real-time with the Hospital Authority. Clinicians should pay special attention to patients with fever or influenza-like illness who visited wet market with live poultry or had contact with poultry in affected areas within the incubation period, that is 10 days before onset.
Letters to doctors, hospitals, kindergartens, child care centres, primary and secondary schools as well as residential care homes for the elderly and the disabled have been issued to alert them to the latest situation.
The case has been notified to the World Health Organization, the National Health and Family Planning Commission (NHFPC), the health authorities of Guangdong and Macau, and the quarantine authority of Shenzhen.
As winter approached, the number of human cases of H7N9 in the Mainland has been increasing. As of yesterday, 16 cases with onsets since September were notified to the CHP by the NHFPC. Based on the seasonal pattern, it is likely that the activity of avian influenza viruses might further increase in winter and heightened vigilance is warranted.
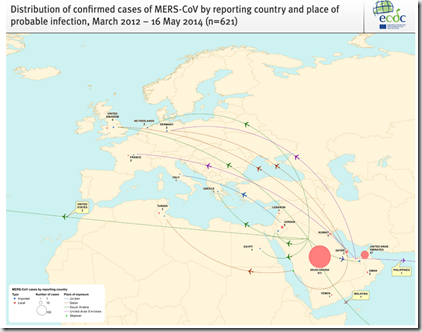
As of yesterday, 470 cases (including at least 184 deaths) have been reported since March 2013, including 454 cases in the Mainland and 16 cases exported to Hong Kong (eleven cases), Taiwan (four cases) and Malaysia (one case).
Enhanced port health measures
-----------------------------
All boundary control points have implemented health surveillance measures. Thermal imaging systems are in place for body temperature checks of inbound travellers. Suspected cases will be immediately referred to public hospitals for follow-up. The DH's Port Health Office has enhanced body temperature checks by handheld devices.
Regarding health education for travellers, the display of posters and broadcasting of health messages in departure and arrival halls, environmental health inspection and provision of regular updates to the travel industry and other stakeholders will be enhanced.
Risk communication
------------------
The CHP's hotline (2125 1111) for public enquiries has been set up and will operate from 9am to 6pm today and tomorrow. The CHP's main page (www.chp.gov.hk/en) has been updated with the activation of the SRL.
Travellers, especially those returning from avian influenza-affected areas with fever or respiratory symptoms, should immediately wear masks, seek medical attention and reveal their travel history to doctors. Healthcare professionals should pay special attention to patients who might have had contact with poultry, birds or their droppings in affected areas.
The public should remain vigilant and take heed of the advice against avian influenza below:
- * Do not visit live poultry markets and farms. Avoid contact with poultry, birds and their droppings;
- If contact has been made, thoroughly wash hands with soap;
- Avoid entering areas where poultry may be slaughtered and contact with surfaces which might be contaminated by droppings of poultry or other animals;
- Poultry and eggs should be thoroughly cooked before eating;
- Wash hands frequently with soap, especially before touching the mouth, nose or eyes, handling food or eating; after going to the toilet or touching public installations or equipment (including escalator handrails, elevator control panels and door knobs); and when hands are dirtied by respiratory secretions after coughing or sneezing;
- Cover the nose and mouth while sneezing or coughing, hold the spit with a tissue and put it into a covered dustbin;
- Avoid crowded places and contact with fever patients; and
- Wear masks when respiratory symptoms develop or when taking care of fever patients.
The public may visit pages below for more information:
- The CHP's avian influenza page (www.chp.gov.hk/en/view_content/24244.html); and
- Global statistics and affected areas of avian influenza in the CHP's website
(www.chp.gov.hk/files/pdf/global_statistics_avian_influenza_e.pdf).
Ends/Sunday, December 28, 2014
Issued at HKT 20:02