# 9990
In early 2012 World Health Director-General Margaret Chan expressed a dire warning about our dwindling antibiotic arsenal (see Chan: World Faces A `Post-Antibiotic Era’) – a sentiment echoed a year later by CDC Director Dr. Thomas Frieden during the release of a major US report on the threat (see McKenna On CDC Antibiotic Resistance Report).
Inevitable conclusions backed up by a long list studies showing the inexorable erosion of our current cache of antibiotics. Some of these reports I’ve covered in the past include:
EID Journal: Acquisition of Drug Resistant Genes Through International Travel
The Lancet: Antibiotic Resistance - The Need For Global Solutions
UK CMO: Antimicrobial Resistance Poses `Catastrophic Threat’
MMWR Vital Signs: Carbapenem-Resistant Enterobacteriaceae (CRE)
Despite decades of warnings, better stewardship of our dwindling antibiotic resources has been slow in coming, even as the number of resistant bacteria continue to grow.
In many countries antibiotics are still available freely (and cheaply) over the counter, public awareness of the risks is low, and surveillance for resistant infections is either low, or non-existent.
Today the World Health Organization released a report, that – while finding some glimmers of hope - nonetheless paints a picture of an international community that is either not really engaged, or lacks the resources, to effectively fight antibiotic resistance.
Of 194 member nations, nearly 1/3rd (n=61) did not respond to this two-year survey conducted by the WHO, leaving huge gaps in the data. Participation was highest in the South East Asian Region (100%) and lowest in the Africa Region (17%).
Results from individual countries are not published, instead combined data is presented for each of the six WHO regions. First links to the full report and the executive summary, followed by some excerpts from the press release.
Publication details
Number of pages: 42
Publication date: 29 April 2015
Languages: English
ISBN: 978 92 4 156494 6
WHO reference number: WHO/HSE/PED/AIP/2015.1Downloads
WHO report finds systems to combat antibiotic resistance lacking in all regions of the world
29 April 2015 Ç€ GENEVA – A quarter of countries that responded to a World Health Organization (WHO) survey have national plans to preserve antimicrobial medicines like antibiotics, but many more countries must also step up. A new report, Worldwide country situation analysis: Response to antimicrobial resistance, which outlines the survey findings, reveals that while much activity is underway and many governments are committed to addressing the problem, there are major gaps in actions needed across all six WHO regions to prevent the misuse of antibiotics and reduce spread of antimicrobial resistance.
“This is the single greatest challenge in infectious diseases today,” says Dr Keiji Fukuda, WHO’s Assistant Director-General for Health Security. “All types of microbes—including many viruses and parasites—are becoming resistant to medicines. Of particularly urgent concern is the development of bacteria that are progressively less treatable by available antibiotics. This is happening in all parts of the world, so all countries must do their part to tackle this global threat.”
Issued a year after WHO’s first report on the extent of antimicrobial resistance globally, which warned of a ‘post-antibiotic era’, this survey—which was completed by 133 countries in 2013 and 2014—is the first to capture governments’ own assessments of their response to resistance to antimicrobial medicines used to treat conditions such as bloodstream infections, pneumonia, tuberculosis (TB), malaria and HIV. It summarizes current practices and structures aimed to address the issue, and shows there are significant areas for improvement.
“While there is a lot to be encouraged by, much more work needs to be done to combat one of the most serious global health threats of our time,” says Dr Fukuda. “Scientists, medical practitioners and other authorities including WHO have been sounding the warning of the potentially catastrophic impact of ignoring antibiotic resistance. Today, we welcome what has been achieved so far, but much more needs to be done to avoid losing the ability to practise medicine and treat both common and serious illnesses.”Key findings of the report include:
- Few countries (34 out of 133 participating in the survey) have a comprehensive national plan to fight resistance to antibiotics and other antimicrobial medicines.
- Monitoring is key for controlling antibiotic resistance, but it is infrequent. In many countries, poor laboratory capacity, infrastructure and data management are preventing effective surveillance, which can reveal patterns of resistance and identify trends and outbreaks.
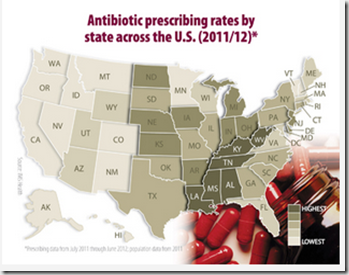
- Sales of antibiotics and other antimicrobial medicines without prescription remain widespread, with many countries lacking standard treatment guidelines, increasing the potential for overuse of antimicrobial medicines by the public and medical professionals.
- Public awareness of the issue is low in all regions, with many people still believing that antibiotics are effective against viral infections.
- Lack of programmes to prevent and control hospital-acquired infections remains a major problem.
While we worry about the sudden emergence of a novel pathogen that could sweep across the globe killing millions, we already have a slow rolling pandemic of antibiotic resistance, which is only growing more dire by the year.
The WHO’s updated factsheet on Antibiotic resistance shows just some of these impacts.
Fact sheet N°194
Updated April 2015Key facts
- Antimicrobial resistance threatens the effective prevention and treatment of an ever-increasing range of infections caused by bacteria, parasites, viruses and fungi.
- It is an increasingly serious threat to global public health that requires action across all government sectors and society.
- Antimicrobial resistance is present in all parts of the world. New resistance mechanisms emerge and spread globally.
- In 2012, WHO reported a gradual increase in resistance to HIV drugs, albeit not reaching critical levels. Since then, further increases in resistance to first-line treatment drugs were reported, which might require using more expensive drugs in the near future.
- In 2013, there were about 480 000 new cases of multidrug-resistant tuberculosis (MDR-TB). Extensively drug-resistant tuberculosis (XDR-TB) has been identified in 100 countries. MDR-TB requires treatment courses that are much longer and less effective than those for non-resistant TB.
- In parts of the Greater Mekong subregion, resistance to the best available treatment for falciparum malaria, artemisinin-based combination therapies (ACTs), has been detected. Spread or emergence of multidrug resistance, including resistance to ACTs, in other regions could jeopardize important recent gains in control of the disease.
- There are high proportions of antibiotic resistance in bacteria that cause common infections (e.g. urinary tract infections, pneumonia, bloodstream infections) in all regions of the world. A high percentage of hospital-acquired infections are caused by highly resistant bacteria such as methicillin-resistant Staphylococcus aureus (MRSA) or multidrug-resistant Gram-negative bacteria.
- Treatment failures due to resistance to treatments of last resort for gonorrhoea (third-generation cephalosporins) have been reported from 10 countries. Gonorrhoea may soon become untreatable as no vaccines or new drugs are in development.
- Patients with infections caused by drug-resistant bacteria are generally at increased risk of worse clinical outcomes and death, and consume more health-care resources than patients infected with the same bacteria that are not resistant.
All of which means it is hard to overstate the seriousness of the problem, or the consequences to humanity should we fail to adequately address it.