Geographic Range of Nipah, Hendra, and fruit bats of the Pteropodidae family – Credit WHO
# 8782
In 2011, in NIH: Investigating A Potential Treatment For Hendra & Nipah Viruses we looked at research using the human monoclonal antibody (hmAb) m102.4 to protect African green monkeys (AGMs) against a Hendra Virus challenge. Twelve subjects were infused with a 100-mg dose of m102.4 beginning at either 10, 24, or 72 hours after infection and again about 48 hours later.
All twelve primates that received the antibodies survived, while all control subjects died by day 8.
The results were so promising, Australian health officials requested m102.4 for emergency use in a woman and her 12-year-old daughter who had been exposed to a horse with the Hendra virus in 2010. Both the woman and child survived and showed no side effects from the treatment (cite).
Similarly, in 2009, research published in PLoS Pathogens illustrated its protective effect against Nipah in ferrets (see A Neutralizing Human Monoclonal Antibody Protects against Lethal Disease in a New Ferret Model of Acute Nipah Virus Infection).
Monoclonal antibodies would not work like a vaccine and confer long-term protection. Instead, a single injection (or series of injections) is hoped to serve as a treatment, or to work as a temporary (several week) prophylaxis.
While the research above was promising, most of these studies involved starting treatment before, or just shortly after, infection, an unrealistic scenario for most therapeutic uses.
Today, we’ve a new study – conducted by University of Texas Medical Branch at Galveston, the Uniformed Services University of the Health Sciences at Bethesda, MD and three NIH Labs (2 at Hamilton, MT & 1 Frederick, MD) - that shows impressive results (on non-human primates, anyway), even when therapy is started 5 days post exposure.
Science Translational Medicine
INFECTIOUS DISEASE
Thomas W. Geisbert1,2,*,†, Chad E. Mire1,2,*, Joan B. Geisbert1,2, Yee-Peng Chan3, Krystle N. Agans1,2, Friederike Feldmann4, Karla A. Fenton1,2, Zhongyu Zhu5, Dimiter S. Dimitrov5, Dana P. Scott4, Katharine N. Bossart6, Heinz Feldmann7 and Christopher C. Broder3,†
Abstract
Nipah virus (NiV) is an emerging zoonotic paramyxovirus that causes severe and often fatal disease in pigs and humans.
There are currently no vaccines or treatments approved for human use. Studies in small-animal models of NiV infection suggest that antibody therapy may be a promising treatment. However, most studies have assessed treatment at times shortly after virus exposure before animals show signs of disease.
We assessed the efficacy of a fully human monoclonal antibody, m102.4, at several time points after virus exposure including at the onset of clinical illness in a uniformly lethal nonhuman primate model of NiV disease.
Sixteen African green monkeys (AGMs) were challenged intratracheally with a lethal dose of NiV, and 12 animals were infused twice with m102.4 (15 mg/kg) beginning at either 1, 3, or 5 days after virus challenge and again about 2 days later. The presence of viral RNA, infectious virus, and/or NiV-specific immune responses demonstrated that all subjects were infected after challenge.
All 12 AGMs that received m102.4 survived infection, whereas the untreated control subjects succumbed to disease between days 8 and 10 after infection. AGMs in the day 5 treatment group exhibited clinical signs of disease, but all animals recovered by day 16. These results represent the successful therapeutic in vivo efficacy by an investigational drug against NiV in a nonhuman primate and highlight the potential impact that a monoclonal antibody can have on a highly pathogenic zoonotic human disease.
Copyright © 2014, American Association for the Advancement of Science
Now that this hmAb has been shown effective against the Nipah virus in non-human primates, researchers hope they may have the basis for what will eventually become a viable treatment for these deadly viruses. For a bit more background, the following is an excerpt from a press release from the University of Texas Medical Branch.
Researchers one step closer to countering deadly Nipah virus
June 25, 2014
Human antibody therapy successfully combats virus five days after infection
An interdisciplinary research team from the University of Texas Medical Branch at Galveston, the Uniformed Services University of the Health Sciences and three groups within the National Institutes of Health reports a new breakthrough in countering the deadly Nipah virus. The human monoclonal antibody known as m102.4 is the first effective antiviral treatment for Nipah that has the potential for human therapeutic applications.
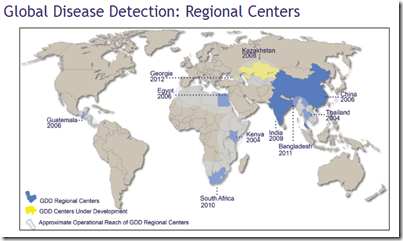
Nipah and the closely related Hendra virus are highly infectious agents that emerged from Pteropid fruit bats in the 1990s, causing serious disease outbreaks in a variety of domestic animals and humans in Australia, Malaysia, Singapore, Bangladesh and India. Recent Nipah outbreaks have resulted in acute respiratory distress syndrome and encephalitis, person-to-person transmission and greater than 90 percent fatality rates among people. These properties make both Nipah and Hendra viruses a concern to human and livestock health.
For some other blogs on the development, and testing of monoclonal antibodies, you may wish to revisit:
- In 2009 in Research: Monoclonal Antibodies Against Influenza researchers at the Dana-Farber Cancer Institute (Dana-Farber), Burnham Institute for Medical Research (Burnham) and the Centers for Disease Control and Prevention (CDC) announced the identification of human monoclonal antibodies (mAb) that work against a wide range of influenza viruses, including the H5N1 bird flu virus.
- And in 2010, in Monoclonal Antibodies Revisited, we looked a Korean company (Celltrion) working on Human Monoclonal Antibodies (moAb) that are designed to work against a wide variety of influenza viruses.