Photo Credit CDC
# 8162
By now, just about everyone has read or heard about the tragic story of the young nurse who died in Canada from the H5N1 virus after returning from a 3-week trip to China. Today ProMed Mail has published a detailed accounting of her signs and symptoms, and clinical treatment, in the days leading up to her death (h/t @HelenBranswell).
Due to its length I won’t try to excerpt the report, but will instead invite you to read it in its entirety at http://www.promedmail.org/direct.php?id=2167282, after you return, I’ll have more on atypical flu presentations.
When we think of flu, the early symptoms are generally cough, fever, and body aches. While this patient had a fever, and eventually developed respiratory symptoms (shortness of breath) and pneumonia, she did not initially present with a cough and her overall appearance was not what you would expect with an influenza patient.
Her `atypical’ symptoms included chest pain, a mild headache (exacerbated by head movement), right upper quadrant and epigastric pain, and nausea and vomiting. And so her initial diagnosis was bacterial pneumonia (based on x-rays), and after her neurological signs appeared, meningococcal encephalitis was also considered.
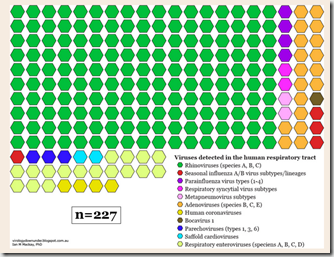
Although influenza is primarily thought of as a respiratory infection, in recent years we’ve seen growing evidence that both seasonal and novel flu stains can manifest in a variety of unusual ways. Neurological and gastrointestinal symptoms – while not typical – are not all that uncommon.
So today, a review of some of those reports from the past few years. As you’ll see, flu comes in many guises, and it isn’t always easy to diagnose.
One of the earliest indications that H5N1 could produce serious (even fatal) non-respiratory illness came from this study involving the deaths of a brother and sister in Vietnam in 2004.
Fatal avian influenza A (H5N1) in a child presenting with diarrhea followed by coma.
de Jong MD, Bach VC, Phan TQ, Vo MH, Tran TT, Nguyen BH, Beld M, Le TP, Truong HK, Nguyen VV, Tran TH, Do QH, Farrar J.
Abstract
In southern Vietnam, a four-year-old boy presented with severe diarrhea, followed by seizures, coma, and death. The cerebrospinal fluid contained 1 white cell per cubic millimeter, normal glucose levels, and increased levels of protein (0.81 g per liter). The diagnosis of avian influenza A (H5N1) was established by isolation of the virus from cerebrospinal fluid, fecal, throat, and serum specimens. The patient's nine-year-old sister had died from a similar syndrome two weeks earlier. In both siblings, the clinical diagnosis was acute encephalitis. Neither patient had respiratory symptoms at presentation. These cases suggest that the spectrum of influenza H5N1 is wider than previously thought.
In June of 2007, we saw a report (see Atypical Presentations of H5N1) out of Indonesia, of a 3-year old child infected with H5N1 but that presented with fever, but without respiratory symptoms. Surprising since fever, cough, and in most cases pneumonia, are pretty much a hallmark the H5N1 virus.
Gastrointestinal symptoms have been reported in a number of H5N1 cases as well, as we saw in 2008 in this large review of Chinese bird flu patients (see Clinical Case Review Of 26 Chinese H5N1 Patients).
And in 2010, we saw a study (see H5N1 Can Replicate In Human Gut) that provided even more evidence that the bird flu virus can thrive outside the human respiratory system. From a Journal of Infectious Diseases brief:
DOI: 10.1086/651457
BRIEF REPORT
Avian Influenza A(H5N1) Viruses Can Directly Infect and Replicate in Human Gut Tissues
Yuelong Shu, Chris Ka‐fai Li, Zi Li, Rongbao Gao, Qian Liang, Ye Zhang, Libo Dong, Jiangfang Zhou, Jie Dong, Dayan Wang, Leying Wen, Ming Wang, Tian Bai, Dexin Li, Xiaoping Dong, Hongjie Yu, Weizhong Yang, Yu Wang,Zijian Feng, Andrew J. McMichael,3 and Xiao‐Ning Xu3
The human respiratory tract is a major site of avian influenza A(H5N1) infection. However, many humans infected with H5N1 present with gastrointestinal tract symptoms, suggesting that this may also be a target for the virus.
In this study, we demonstrated that the human gut expresses abundant avian H5N1 receptors, is readily infected ex vivo by the H5N1 virus, and produces infectious viral particles in organ culture.
An autopsy colonic sample from an H5N1infected patient showed evidence of viral antigen expression in the gut epithelium. Our results provide the first evidence, to our knowledge, that H5N1 can directly target human gut tissues.
In 2009, in Study: H5N1 Infection And Brain Damage, we looked at a story by Maggie Fox – who was then writing for Reuters – on a PNAS study that found the H5N1 virus was neurotropic (able to infect & damage nerve cells) . . . at least in mice.
Bird flu causes Alzheimer's-like brain damage, study says
Tests on mice infected with H5N1 virus show lasting damage to nerve cells, including the brain
Maggie Fox
Washington — Reuters News Agency Last updated on Monday, Aug. 10, 2009 05:13PM EDT
Survivors of bird flu, and perhaps other influenza viruses, may not be out of the woods once the fever and cough are gone: Animal studies suggest the virus may damage the brain and cause Alzheimer's and Parkinson's disease.
The tests on mice show that the H5N1 virus can get into the brain, causing damage that resembles Parkinson's and Alzheimer's in humans, the researchers wrote in the Proceedings of the National Academy of Sciences.
“Our results suggest that a pandemic H5N1 pathogen, or other neurotropic influenza virus, could initiate central nervous system disorders of protein aggregation including Parkinson's and Alzheimer's diseases,” Richard Smeyne of St. Jude Children's Research Hospital in Memphis, Tenn., and colleagues wrote.
(Continue . . . )
Another article on this research, published on the St. Jude Children’s Research Hospital website:
At least one strain of the H5N1 avian influenza virus leaves survivors at significantly increased risk for Parkinson’s disease and possibly other neurological problems later in life, according to new research from St. Jude Children’s Research Hospital.
(Continue . . . )
This PNAS study (link below) found that the H5N1 virus was highly neurotropic in lab mice, and in the words of the authors `could initiate CNS disorders of protein aggregation including Parkinson's and Alzheimer's diseases’.
Highly pathogenic H5N1 influenza virus can enter the central nervous system and induce neuroinflammation and neurodegeneration
Haeman Jang, David Boltz, Katharine Sturm-Ramirez, Kennie R. Shepherd, Yun Jiao, Robert Webster and Richard J. Smeyne
It isn’t just H5N1 that presents in atypical fashion, as we saw last October in CMJ: Varied Clinical Presentations Of H7N9. This study reviewed the case of an 87 year-old man who initially (April 4th) complained of loss of appetite and strength but no fever, cough, or expectoration.
Chest x-rays on the 6th indicated some lung inflammation, but due to his symptoms a bacterial, not a viral cause, was suspected. He admitted to the hospital and was placed on antibiotics (cefuroxime).
Five days into his illness, he developed dyspnea (shortness of breath) and an elevated temperature, and on April 10th deteriorated further. Influenza was finally suspected, and he was started on oseltamivir and levofloxacin, and a decision to test for H7N9 was made.
Despite ICU treatment, and a transfer to specialized hospital, the patient died on April 21st.
The authors wrote:
This case history serves to remind us that we need timely use of antiviral treatment, even for the patients whose clinical manifestations are not typical but whose lung inflammation may be developing rapidly. Careful clinical observation needs to be carried out so that appropriate treatment can begin as early as possible and progression culminating in death is minimized
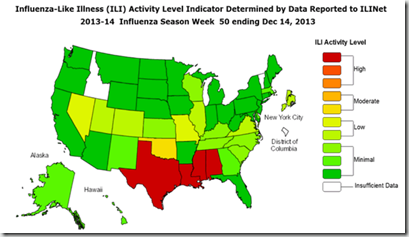
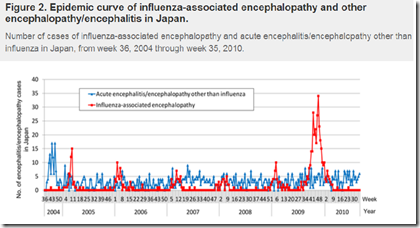
During the opening months of the 2009 H1N1 pandemic, we also saw a number of influenza-related encephalopathies.
Encephalopathy isn’t a distinct disease, but rather refers to a syndrome of diffuse brain dysfunctions, which may be associated with a variety of causes (including viral, bacterial, trauma, prions, and toxic chemicals).
The overriding hallmark of encephalopathy is an altered mental state, although depending and severity of encephalopathy, common neurological symptoms such as progressive memory loss and changes in cognitive ability, personality changes, inability to concentrate, lethargy, seizures and loss of consciousness may be seen.
Barely 90 days after the novel H1N1 virus emerged, the CDC’s MMWR reported on 4 pediatric patients with the novel H1N1 virus who presented with neurological symptoms including unexplained seizures and altered mental status:
Additional reports came in over the summer and fall, particularly from Japan, indicating an unusual number cases of Influenza-related encephalopathy (IAE) among children (see Japan: Influenza Related Encephalopathy).
In January of 2010, the CDC’s EID Journal carried a report called Neurologic Manifestations of Pandemic (H1N1) 2009 Virus Infection and in September, the Annals of Neurology carried a study called Heightened Neurologic Complications in Children with Pandemic H1N1 Influenza that found:
The most common neurological complications exhibited with novel H1N1 were seizures (12 patients or 67%), with seven exhibiting status epilepticus, a potentially life-threatening condition involving continuous or recurrent seizures that can last for a half hour or longer.
The mean age of children admitted with neurological symptoms from H1N1 was more than twice the age (6.5 years) than usually seen with seasonal flu (2.4 years).
Over the past 15 years Influenza has been increasingly recognized as a rare cause of encephalopathy. For reasons not understood, it is reported most often among children and adolescents in Japan and Taiwan.
Another example of how influenza may impact systems outside of our respiratory tract, in Revisiting The Influenza-Parkinson’s Link we looked at a study conducted by the University of British Columbia, that found a linkage between a past history of severe bouts of influenza and the likelihood of developing Parkinson’s disease later in life.
In fact, according to their research, a severe bout of influenza doubles a person’s chances of developing the neurological condition. Interestingly, the UBC researchers found that those who caught red measles as a child were 35% less likely to develop the disabling disease.
The article appears in the journal Movement Disorders, and the abstract may be read at:
M. Anne Harris PhD, Joseph K. Tsui MB, Stephen A. Marion MD, Hui Shen PhD, Kay Teschke PhD
During the 1918 pandemic, and the decade that followed, more than a million people around the world were afflicted by a mysterious neurological disorder called Encephalitis Lethargica (EL), which some researchers suspect may have been part of some long-term sequelae of the virus.
While most researchers now believe that EL and Spanish influenza pandemic were not etiologically linked, in The relationship between encephalitis lethargica and influenza: A critical analysis Sherman McCall, Joel A Vilensky and Jeffery K Taubenberger looked at both sides of this longstanding debate.
Quite interestingly, they conclude:
Empirical studies provide little evidence of influenza causation; but, as we have demonstrated, technical limitations and the shortage of appropriate material for testing limit the degree of confidence. Therefore, unless another cause of classical EL is positively identified, its return in the context of another influenza pandemic remains formally possible. Such a recurrence would provide an opportunity to establish the etiology of EL using modern methods.
In light of the recent research linking Parkinson’s and influenza, this linkage – while far from proven – would seem at least plausible.
As far as where this meandering through the archives leaves us, I suppose it should be with greater respect for such a versatile and highly adaptive virus. One that can produce such a wide range of symptoms (and severity), both in terms of an acute infection - and potentially - in the form of long term sequelae like Parkinson’s or narcolepsy.
Frankly, the longer I blog about influenza, the more impressed I am with its capabilities.