Credit Texas Influenza Weekly Surveillance
# 8097
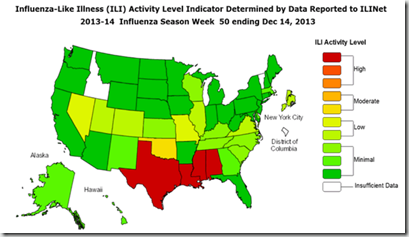
While some in the media this week are hyping the recent influenza deaths in Texas (see Texas DSHS Statement On Recent Spike In Flu Activity) as the `Return of Swine Flu’, the reality is, the virus never left.
It has been with us since it first emerged in 2009, but has taken a backseat to the other seasonal strain - H3N2 - in North America over the past couple of years.
While H1N1 is no longer a pandemic virus, it can still pack a punch . . . particularly for those under the age of 65, and those with pre-existing medical conditions. And since it hasn’t been the dominant strain in North America the past couple of years, many people have reduced immunity to it (particularly if they skipped the flu shot).
This week we’ve seen reports of multiple deaths in Texas, and around the nation, now attributed to the H1N1 virus. Many others have been hospitalized with severe illness.
Yesterday, the Texas DSHS sent out a notice to doctors and hospitals advising them on how to test for, and treat, severe cases of flu.
TEXAS DEPARTMENT OF STATE HEALTH SERVICES
DAVID L. LAKEY, M.D. COMMISSIONER
www.dshs.state.tx.us
**INFLUENZA HEALTH ALERT**
December 20, 2013
Dear Colleague:
Statewide influenza-like illness (ILI) activity continues to increase and is above baseline levels. ILI intensity is high in Texas, and influenza is now widespread. All Texas regions have reported laboratory confirmed influenza. Over 90% of positive influenza tests reported from Texas laboratories have been typed as influenza A. Of those influenza A viruses that have been subtyped, 90% have been the 2009 pandemic H1N1 subtype. This subtype of influenza is included in this season's influenza vaccine.
No novel influenza cases have been reported in Texas.
No antiviral resistant influenza strains have been reported in Texas.
Encourage patients to get vaccinated for influenza.
Clinicians should consider antivirals even if the Rapid Influenza Diagnostic Test is negative.
Background: Influenza viruses can be spread by large respiratory droplets generated when an infected person coughs or sneezes in close proximity to an uninfected person. Symptoms can include fever, dry cough, sore throat, headache, body aches, fatigue, and nasal congestion. Among children, otitis media, nausea, vomiting, and diarrhea are common.
Most people generally recover from illness in 1-2 weeks, but some people develop complications and may die from influenza. The highest rates of influenza infection occur among children; however, the risks for serious health problems, hospitalizations, and deaths from influenza are higher among people 65 years of age or older, very young children, and people of any age who have medical conditions that place them at increased risk for complications from influenza (see Treatment).
Vaccination: Everyone who is at least 6 months of age should get a flu vaccine this season. It is not too late for vaccination. There are several flu vaccine options available for the 2013-2014 flu season. All these vaccines contain the currently circulating H1N1 strain. DSHS does not recommend one flu vaccine over another, although there are special indications for some (such as a high-dose inactivated trivalent vaccine approved for persons age 65 years and older).
The 2013-2014 trivalent influenza vaccine is made from the following three
An A/California/7/2009 (H1N1)pdm09-like virus
An A(H3N2) virus antigenically like the cell-propagated prototype virus A
A B/Massachusetts/2/2012-like virus
Rapid Lab Tests: Rapid Influenza Diagnostic Tests (RIDTs) can be useful to identify influenza virus infection, but false negative test results are common during influenza season. Clinicians should be aware that a negative RIDT result does NOT exclude a diagnosis of influenza in a patient with suspected influenza. When there is clinical suspicion of influenza and antiviral treatment is indicated, antiviral treatment should be started as soon as possible, even if the result of the RIDT is negative, without waiting for results of additional influenza testing.
Treatment: Oseltamivir and zanamivir are chemically related antiviral medications known as neuraminidase inhibitors that have activity against both influenza A and B viruses. Early antiviral treatment can shorten the duration of fever and illness symptoms, may reduce the risk of complications and death, and may shorten the duration of hospitalization. Clinical benefit is greatest when antiviral treatment is administered early, especially within 48 hours of influenza illness onset. Decisions about starting antiviral treatment should not wait for laboratory confirmation of influenza.
Antiviral treatment is recommended as early as possible for any patient with confirmed or suspected influenza who:
Is hospitalized.
Has severe, complicated, or progressive illness.
Is at higher risk for influenza complications.
Persons at higher risk for influenza complications recommended for antiviral treatment include:
Children aged younger than 2 years.
Adults aged 65 years and older.
Persons with chronic pulmonary (including asthma), cardiovascular (except hypertension alone), renal, hepatic, or hematological disease (including sickle cell disease); metabolic disorders (including diabetes mellitus); or neurologic and neurodevelopment conditions (including disorders of the brain, spinal cord, peripheral nerve, and muscle such as cerebral palsy, epilepsy [seizure disorders], stroke, intellectual disability [mental retardation], moderate to severe developmental delay, muscular dystrophy, or spinal cord injury). Persons with immunosuppression, including that caused by medications or by HIV infection.
Women who are pregnant or postpartum (within 2 weeks after delivery).
Persons aged younger than 19 years who are receiving long-term aspirin therapy.
American Indians/Alaska Natives.
Persons who are morbidly obese (i.e., body-mass index is equal to or greater than 40).
Residents of nursing homes and other chronic-care facilities.
Clinical judgment, on the basis of the patient's disease severity and progression, age, underlying medical conditions, likelihood of influenza, and time since onset of symptoms, is important when making antiviral treatment decisions for high-risk outpatients.
Additional details regarding antiviral treatment can be found at
http://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm.
Disease Reporting Requirements/Statute: Several Texas laws (Health & Safety Code. Chapters 81, 84, and 87) require specific information regarding notifiable conditions to be provided to DSHS. Health care providers, hospitals, laboratories, schools, childcare facilities and others are required to report patients who are suspected of having a notifiable condition (Chapter 97, Title 25, Texas Administrative Code). In Texas, influenza-associated pediatric mortality is required to be reported within one work day. Clusters or outbreaks of any disease, including influenza, should be reported immediately. Reports of influenza-associated pediatric mortality and influenza or influenza-like illness outbreak should be made to your local health department or to 1-800-705-8868.
David Lakey, M.D.
Commissioner
Texas Department of State Health Services
Some of the initial confusion with the outbreak in Texas came from reports of `negative flu tests’ among some of the patients. As we’ve discussed often in the past, Rapid Influenza Detection Tests are quick and easy – but they aren’t always accurate (see No Doesn’t Always Mean No).
Hence the reminder by the DSHS (and the CDC, btw) that `a negative RIDT result does NOT exclude a diagnosis of influenza’.
For more on the limitations of RIDT tests, you may wish to revisit last year’s side-by-side comparison of 11 commercially available test kits in MMWR: Evaluating RIDTs.
With H1N1 prowling the nation, aided and abetted by H3N2 and Influenza B, it is particularly important to maintain good flu hygiene right now. The CDC recommends:
- Wash your hands often with soap and water or an alcohol-based hand rub.
- Avoid touching your eyes, nose, or mouth. Germs spread this way.
- Try to avoid close contact with sick people.
- Practice good health habits. Get plenty of sleep and exercise, manage your stress, drink plenty of fluids, and eat healthy food.
- Cover your nose and mouth with a tissue when you cough or sneeze. Throw the tissue in the trash after you use it.
- If you are sick with flu-like illness, stay home for at least 24 hours after your fever is gone without the use of fever-reducing medicine.
And if you haven’t already gotten your flu shot, it is certainly not too late to do that as well.