Arthroconidia of Coccidioides immitis – Credit CDC
# 7039
Although viruses and bacteria garner most of the infectious disease headlines, mycotic diseases – caused by pathogenic fungi – produce their fair share of morbidity and mortality across the United States each year as well.
NOTE: While it makes sense to wear a mask in certain high exposure scenarios, environmental fungal spores are ubiquitous, and for the most part there really isn’t very much any of us can do to prevent exposure .
Fortunately, for most people, exposure to these fungi does not result in illness. While anyone can be infected, those who are immunocompromised are at considerably greater risk.
Some percentage of those infected may experience a mild flu-like illness, while an even smaller percent may experience a more serious illness, which can result in pneumonia, soft tissue infections, and (rarely) death.
Last October, in Four Fungal Foes, we looked at four common fungal diseases in North America - but briefly:
Along the Ohio River Valley and across a good deal of the Southeastern United States people are exposed to Histoplasma capsulatum, a fungus which is found in bird and bat droppings, that can cause Histoplasmosis.

Credit Wikipedia
Similarly, Blastomycosis (aka Gilchrist's disease), which is caused by Blastomyces dermatitidis - found in decaying leaves and grass – is widely spread across much of the eastern half of the country.
And in 1999 a tropical fungus called Cryptococcus gattii (a yeast, really) appeared on Vancouver Island. Spread by the wind, it has expanded its range into Washington and Oregon.
C. gattii infection remains rare in the United States, with only about 100 cases diagnosed between 2004 –2011, mostly from Oregon and Washington (cite).
In 2010 the CDC’s Journal of Emerging Infectious Diseases published a research article on the spread of C. gattii in British Columbia (Epidemiology of Cryptococcus gattii, British Columbia, Canada, 1999–2007).
Additional fungal pathogens of concern include:
Aspergillosis, Candidiasis, Dermatophytes, Exserohilium, Fungal Keratitis, Mucormycosis, Pneumocystis pneumonia, Sporotrichosis and others – all of which fall under the purview of the CDC’s Division of Bacterial and Mycotic Diseases, Mycotic Diseases Branch.
But among all of the environmental fungal infections across the United States, the rising star appears to be coccidioidomycosis.
As a native Floridian, I confess I’d never heard of Coccidioidomycosis until I moved to Phoenix in 1975 to work as a paramedic.
Upon my arrival I received a `Welcome to Arizona’ indoctrination that reviewed such local scenarios as as scorpion stings, Gila Monster bites, bubonic plague, sand storms, and `Valley Fever’ . . . aka Coccidioidomycosis.
Coccidioidomycosis is caused by the inhalation of spores from one of two soil borne fungi - Coccidioides immitis or C. posadasii - both commonly found in the American Southwest.
Their spores can remain dormant in the desert soil for years, only to become airborne when the earth is disturbed by farming, earthquakes, construction, or windstorms.
Most of the people who live in regions where these fungi are endemic are eventually exposed and either develop brief asymptomatic infections or mild flu-like symptoms.

Credit Wikipedia
Last fall I highlighted the CDC’s Valley Fever site , which calls `cocci’ a `silent epidemic’, and links to a series of outside investigative reports called “Just One Breath” by the Reporting on Health Collaborative.

It Only Takes One Breath
Areas Where Valley Fever is Endemic
Anyone can get valley fever, including children. However, it is most common among older adults, particularly those 60 and older. People who have recently moved to an area where the disease naturally occurs are at higher risk for infection.
Several groups of people are at higher risk for developing the severe forms of valley fever, including:
-
African Americans
-
Asians
-
Women in their 3rd trimester of pregnancy
-
People with weak immune systems, including those with an organ transplant or who have HIV/AIDS
Yesterday, the CDC’s MMWR carried a report on the skyrocketing rise in Coccidioidomycosis across the American Southwest between 1998 and 2011.
The incidence of detected infection has increased 8-fold over that time, going from 5.4 per 100,000 population in 1998 to 42.6 in 2011.
Some of this increase may well be `artifactual’, as coccidioidomycosis became a `legally reportable’ disease in Arizona in 1997 and protocols for testing, reporting, and surveillance have improved over the years.
But better reporting is unlikely to account for this much of an increase.
First stop, the MMWR report, followed by a link to the CDC press release, and then finally, a 30 minute video from the Arizona Department of Health Services (AZDHS) on `Valley Fever’.
March 29, 2013 / Vol. 62 / No. 12
CE Available
Increase in Reported Coccidioidomycosis — United States, 1998–2011
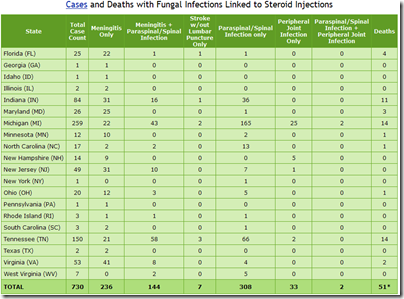
Coccidioidomycosis, also known as valley fever, can be costly and debilitating, with nearly 75% of patients missing work or school because of their illness, and approximately 40% requiring hospitalization. Previous publications have reported state-specific increases in coccidioidomycosis in Arizona and California during 1998–2001 and 2000–2007, respectively. To characterize long-term national trends, CDC analyzed data from the National Notifiable Diseases Surveillance System for the period 1998–2011. This report describes the results of that analysis
(Continue . . .)
From the CDC’s Newsroom.
Valley Fever, a fungal respiratory infection, dramatically increased in several southwestern states from 1998 through 2011, according to a new study by the Centers for Disease Control and Prevention. Cases in Arizona, California, Nevada, New Mexico and Utah rose from 2,265 in 1998 to more than 22,000 in 2011.
Valley Fever (Coccidioidomycosis) is caused by inhaling a fungus called Coccidioides, which lives in the soil in the southwestern United States. Not everyone who is exposed to the fungus gets sick, but those who do typically have flu-like symptoms that can last for weeks or months. More than 40 percent of patients who get ill from Valley Fever may require hospitalization at some point, with an average cost of nearly $50,000 per hospital visit. Previous studies have shown that, of those who get sick, nearly 75 percent miss work or school – for approximately two weeks.
"Valley Fever is causing real health problems for many people living in the southwestern United States," said CDC Director Tom Frieden, M.D., M.P.H. "Because fungus particles spread through the air, it’s nearly impossible to completely avoid exposure to this fungus in these hardest-hit states. It’s important that people be aware of Valley Fever if they live in or have travelled to the southwest United States."
This recent increase in Valley Fever could be related to changes in weather, which could impact where the fungus grows and how much of it is circulating; higher numbers of new residents; or changes in the way the disease is detected and reported to the states or CDC. More research is needed to understand why the number of reported cases of Valley Fever has increased. Between 1998 and 2011, Arizona and California had average increases in Valley Fever incidence of 16 and 13 percent per year, respectively. The CDC has provided grants to these two states to study Valley Fever.
During this time period, nearly 112,000 cases of Valley Fever were reported from 28 states and Washington, D.C., but 66 percent of cases were in Arizona, 31 percent were in California, 1 percent were in Nevada, New Mexico, and Utah, and about 1 percent were in all other states combined.
"It’s difficult to say what’s causing the increase," said Benjamin J. Park, M.D., chief epidemiologist with CDC’s Mycotic Diseases Branch. "This is a serious and costly disease and more research is needed on how to reduce its effects."
(Continue . . .)
For a more local perspective, the AZDHS has a 3-part video called `Valley Fever: The Impact On Arizonans’, produced in 2008.
Part 2 & 3 are available at the following links.
9:03 VF-Web-Part-2.wmv
9:22 VF-Web-Part-3.wmv
And lastly, Robert Roos of CIDRAP NEWS has coverage of this story from last night, called:
CDC: Valley fever cases in US Southwest rising fast