Note: Today is day five of National Hurricane Preparedness Week, and the focus today is on forecasting.
A couple of years ago I took a look at the life of legendary hurricane forecaster Grady Norton, and at how hurricane forecasting technology has changed over the past 50 years.
Today, a (slightly updated) repeat of that column for those who missed it.
# 7340
For those of a certain age who can remember growing up along the Gulf or Atlantic coasts in the 1950’s - before the advent of weather satellites - the technology we have at hand today is truly remarkable.
Our satellites today can probe deep into storm clouds and detect wind speeds, water vapor, precipitation, and heat energy of storm systems a thousand miles from the nearest weather observation post.

Three different views from space, taken May 26th, 2011 1345Z – NOAA
Weather forecasting began a new age when on April 1st 1960, Tiros I - the world's first weather satellite - was launched into Earth orbit from Cape Canaveral, Florida.
For the first time, we had a `god's eye view' of earth. Regions of our globe where once cartographers could only inscribe "Here there be Dragons' could be watched 24 hours a day.
Our view of our world changed, practically overnight.
It was a wondrous day for everyone, except possibly for members of the Flat Earth Society. Below is the first television picture from earth orbit.
I was six years old, and I remember it like it was yesterday.
Sure the pictures were grainy, and the resolution laughable by today's standards, but for the first time we could watch from aloft and observe how and where hurricanes formed.
It meant we were no longer solely dependent on ship's reports and Hurricane Hunter aircraft to know if disaster lay just beyond the horizon.
It meant more than 12 hours warning to prepare for a storm.
TIROS 1 could take and transmit about 1 picture an hour, and only during daylight hours. Infrared capability – which allowed 24 hour coverage - was added to later `birds'.
Today, our reconnaissance satellites can take 40 pictures an hour, and see right through the clouds and measure rainfall, winds and even sea water temperatures. As a result, hurricane forecasting has improved tremendously over the past 50 years.
For those with an interest in how it was done before the advent of weather satellites and supercomputers, I’ve a bit of a treat today.
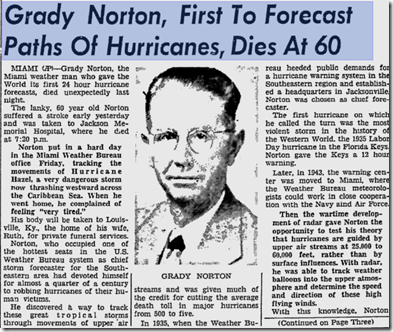
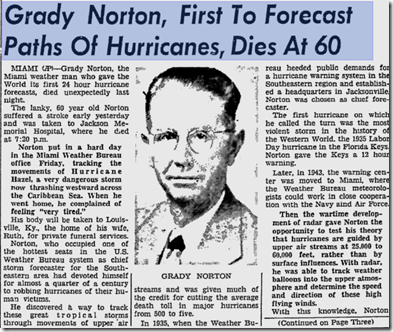
A profile of the first great hurricane forecaster – Grady Norton.
First, during the 1950’s there was a little remembered TV series called The Man Behind The Badge. Hosted by Charles Bickford, the show profiled public servants who had made important contributions to public safety.
In 1955 a dramatized tribute to legendary hurricane forecaster Grady Norton was broadcast. Grady had passed away suddenly of a stroke just a few months before while tracking Hurricane Hazel.
October 10th, 1954 Daytona News-Journal Article.
This 30 minute show stars Milburn Stone (of Gunsmoke Fame), and is hosted by a nostalgia TV site called LIKE Television. It’s a fictionalized story, but I think you’ll find it well worth viewing.
Click the image below to view the show.
I
Norton became the Chief Hurricane Forecaster at the Jacksonville Weather Bureau Hurricane center in 1935 and famously forecast the track of the 200+ MPH Labor Day storm that year, providing 12 critical hours of warning to the Keys and South Florida.

In 1943 the Hurricane forecasting office moved to Miami, as a joint effort of the National Weather Service, Air Force, and Navy. Norton remained their Chief forecaster and most public spokesperson until his death in 1954.
It wasn’t until the mid-1960s that the NHC as we know it today was established as its own entity, separate from the National Weather Service.
While the first director of the National Hurricane Center is listed as Gordon Dunn (1965–1967), Grady Norton is widely regarded as that agency’s first `unofficial’ director.
When meteorologists talk about Grady Norton today, they do so with considerable wonder and awe. His uncanny ability to track storms based on little more than ships reports was the stuff of legend.
While primitive by today’s standards, the work done by Grady Norton and other pioneers of meteorology during the first half of the last century deserves mention and remembrance.
Despite the limited technology of the day, they undoubtedly saved a lot of lives.
For a look at how forecasting is done today, you can watch the following short video from the National Hurricane Center.
Tomorrow, day six of hurricane preparedness week, we’ll be looking at planning for the storm’s arrival. If you haven’t already downloaded the updated Tropical Cyclone Preparedness Guide, now would be an excellent time to do so.