Photo Credit CDC EID Journal
# 7864
Over the past several months a newly emerging coronavirus – PEDV – has been identified in the United States, affecting swine herds in at least 17 states, resulting in high mortality, particularly in piglets. The virus was first identified in the United States in May of this year, but there have been reports of the virus both in Asia and in Europe, going back several decades.
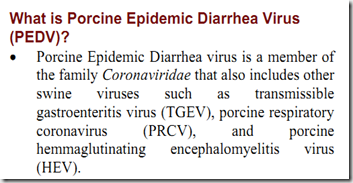
The University of Minnesota’s Center for Animal Health and Food Safety describes the virus thusly:
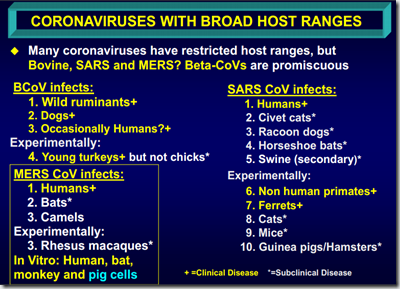
With the recent emergence of another coronavirus – MERS-CoV – and the history of human epidemic sparked by the SARS coronavirus a decade ago, there is understandable interest in PEDV both by agricultural and public health interests.
It should be quickly noted, however, that we’ve seen no evidence of human infection due to PEDV coronavirus, so PEDV is not considered a zoonotic disease.
While SARS and MERS are both betacoronaviruses, PEDV is an alphacoronavirus (two other genera also exist, Gammacoronavirus, and Deltacoronavirus). The first two (alpha & beta) are believed to originate in bats (but are found in many other species), with the second two (Gamma & Delta) are believed to have an avian origin.
Although PED (porcine epidemic diarrhea) has been recognized in Asia since the 1970s, it has been considered exotic in North America. Starting around 2010, China reported a sudden increase related pig deaths, which was the subject of the following CDC’s EID Journal dispatch published in August of 2012.
New Variants of Porcine Epidemic Diarrhea Virus, China, 2011
Wentao Li, Heng Li, Yunbo Liu, Yongfei Pan, Feng Deng, Yanhua Song, Xibiao Tang, and Qigai He
Abstract
In 2011, porcine epidemic diarrhea virus (PEDV) infection rates rose substantially in vaccinated swine herds. To determine the distribution profile of PEDV outbreak strains, we sequenced the full-length spike gene from samples from 9 farms where animals exhibited severe diarrhea and mortality rates were high. Three new PEDV variants were identified.
<SNIP>
The first confirmed PED case in the People’s Republic of China was reported in 1973. Almost 2 decades later, an oil emulsion, inactivated vaccine was developed and has since been in wide use throughout the swine industry in China. Until 2010, the prevalence of PEDV infection was relatively low with only sporadic outbreaks; however, starting in late 2010, a remarkable increase in PED outbreaks occurred in the pig-producing provinces.
(Continue . . . )
All of which serves as prelude to a study, published yesterday in the open access journal mBio, that takes a detailed look at the:
Origin, Evolution, and Genotyping of Emergent Porcine Epidemic Diarrhea Virus Strains in the United States
Yao-Wei Huanga,b, Allan W. Dickermanc, Pablo Piñeyroa, Long Lid, Li Fangd, Ross Kiehnee, Tanja Opriessnigf,g, Xiang-Jin Menga
ABSTRACT
Coronaviruses are known to infect humans and other animals and cause respiratory and gastrointestinal diseases. Here we report the emergence of porcine epidemic diarrhea virus (PEDV) in the United States and determination of its origin, evolution, and genotypes based on temporal and geographical evidence. Histological lesions in small intestine sections of affected pigs and the complete genomic sequences of three emergent strains of PEDV isolated from outbreaks in Minnesota and Iowa were characterized. Genetic and phylogenetic analyses of the three U.S. strains revealed a close relationship with Chinese PEDV strains and their likely Chinese origin. The U.S. PEDV strains underwent evolutionary divergence, which can be classified into two sublineages. The three emergent U.S. strains are most closely related to a strain isolated in 2012 from Anhui Province in China, which might be the result of multiple recombination events between different genetic lineages or sublineages of PEDV. Molecular clock analysis of the divergent time based on the complete genomic sequences is consistent with the actual time difference, approximately 2 to 3 years, of the PED outbreaks between China (December 2010) and the United States (May 2013).
The finding that the emergent U.S. PEDV strains share unique genetic features at the 5′-untranslated region with a bat coronavirus provided further support of the evolutionary origin of PEDV from bats and potential cross-species transmission. The data from this study have important implications for understanding the ongoing PEDV outbreaks in the United States and will guide future efforts to develop effective preventive and control measures against PEDV.
IMPORTANCE The sudden emergence of porcine epidemic diarrhea virus (PEDV), a coronavirus, for the first time in the United States causes significant economic and public health concerns. Since its recognition in May 2013, PEDV has rapidly spread across the United States, resulting in high mortality in piglets in more than 17 States now.
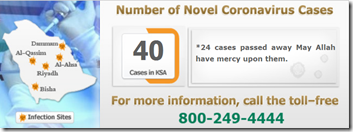
The ongoing outbreaks of Middle East respiratory syndrome coronavirus in humans from countries in or near the Arabian Peninsula and the historical deadly nature of the 2002 outbreaks of severe acute respiratory syndrome coronavirus create further anxiety over the emergence of PEDV in the United States due to the lack of scientific information about the origin and evolution of this emerging coronavirus.
Here we report the detailed genetic characterization, origin, and evolution of emergent PEDV strains in the United States. The results provide much needed information to devise effective preventive and control strategies against PEDV in the United States.
<SNIP>
In summary, we report here the emergence of PEDV in the United States and detailed genetic and phylogenetic analyses of the complete genomic sequences of three emergent U.S. PEDV strains from Minnesota and Iowa. The findings that the emergent U.S. PEDV strains are most closely related to Chinese G2a strains suggest that the emergence of the PEDV in the United States likely originated from China. However, the exact source of the origin is difficult to identify at this point. The finding that the emergent PEDV strains in the United States share unique genetic features with a bat coronavirus further suggests a possible evolutionary origin of PEDV from bat species and potential cross-species transmission. The information presented in this study will guide the current control measures to stop the ongoing spread of PEDV in the United States and also provides important clues for the development of an effective vaccine against the emergent PEDV strains.
(Continue . . . )
Whether the result of an introduction from China, or evolutionary events here in the United States, pig producers are now confronted with at least three new variants of this virus. PEVD has the potential to cause extensive economic damage to pork producers across the nation.
It is just one of the many coronaviruses that affect animals species, but thankfully, not humans.
Other non-zoonotic coronaviruses include Infectious bronchitis virus (IBV) in birds, (TEGV) transmissible gastroenteritis in swine, Bovine coronavirus (BCV), Feline coronavirus (FCoV), canine coronavirus (CCoV), and coronaviruses that target turkeys and ferrets.
The rub, as always, is that viruses are moving targets. As we’ve just seen, a number of new variants have appeared here in the United States and in China over the past three years. None have shown any signs of infecting humans, but until 2012, we’d never seen evidence of the MERS-CoV jumping species either.
Which illustrates the importance of good surveillance and testing of livestock for infectious diseases, even those that don’t currently pose a threat to human health.
Because with viruses, an unexpected change in behavior can be literally only a few mutations away.