# 8788
This week’s Eurosurveillance bonanza of avian flu transmission & evolution papers has more than enough good stuff to keep us busy reading for hours. All of these papers are of great interest, but one in particularly grabbed my attention, mainly due to the potential impact of its findings.
A study that looks at the continual evolution of the H7N9 virus in Mainland China.
To recap: in February of last year a new and dangerous avian influenza virus (H7N9) jumped to humans in Eastern China, although we did not learn about it until the end of March (see More Details Emerge On Shanghai H7N9 Case). Unlike many of the other avian influenza viruses we’ve seen - this virus produced no visible signs of illness in poultry - making it particularly difficult to detect and control.
Benign in poultry, but not in humans, H7N9 often produces a severe form of pneumonia. One that has killed roughly 30% of those known to have been infected.
The only saving grace has been this virus has not yet achieved the ability to transmit efficiently from one human to another. The vast majority of human cases appear to be the result of direct exposure to infected birds or to their environment.
In that first wave about 130 human cases emerged, tapering off only after aggressive controls on live bird markets were imposed in April and May of 2013 (see The Lancet: Poultry Market Closure Effect On H7N9 Transmission). After a quiescent summer, colder fall and winter temperatures brought with it a resurgence in the number of human cases, with the second wave roughly double the size of the first (cite).

Two Waves of H7N9 - Credit Hong Kong’s CHP
A month ago, in EID Journal: H7N9 As A Work In Progress, we looked at a study that found the H7N9 avian virus continues to reassort with local H9N2 viruses, making the H7N9 viruses that circulated in wave 2 genetically distinct from those that were seen during the 1st wave.
As we’ve discussed before, the genetic contributions from the avian H9N2 virus appear to be significant.
Of the three avian flu viruses we are currently watching with the most concern – H5N1, H7N9, and H10N8 – all share several important features (see Study: Sequence & Phylogenetic Analysis Of Emerging H9N2 influenza Viruses In China):
- They all first appeared in Mainland China
- They all have come about through viral reassortment in poultry
- And most telling of all, while their HA and NA genes differ - they all carry the internal genes from the avian H9N2 virus
It turns out the relatively benign and ubiquitous H9N2 is actually a fairly promiscuous virus, as bits and pieces of it keep turning up in new reassortant viruses. See PNAS: Reassortment Of H1N1 And H9N2 Avian viruses & PNAS: Reassortment Potential Of Avian H9N2 for some earlier looks at H9N2’s active social life.
Today, in research from a group of scientists working for China’s National and Provincial CDCs, we learn that the genetic diversity of the H7N9 virus is even greater than previously described, and that continual reassortment with the H9N2 virus, along with passage through a variety of host species, appears to be influencing its ongoing evolution.
A process the authors call `genetic tuning’.
Non-scientists will likely find this article tough sledding (parts certainly were for me), as it is more than a little technical. It is, however, a fascinating paper.
With apologies in advance to any real scientists who may be reading this - come back after the link and abstract - and I’ll do my best to hack through some of the tall grass and go over a few of the highlights.
Eurosurveillance, Volume 19, Issue 25, 26 June 2014
Research articles
Genetic tuning of the novel avian influenza A(H7N9) virus during interspecies transmission, China, 2013
D Wang1,2, L Yang1,2, R Gao1, X Zhang3, Y Tan4, A Wu5, W Zhu1, J Zhou1, S Zou1, Xiyan Li1, Y Sun6, Y Zhang7, Y Liu8, T Liu9, Y Xiong10, J Xu11, L Chen12, Y Weng13, X Qi14, J Guo1, Xiaodan Li1, J Dong1, W Huang1, Y Zhang1, L Dong1, X Zhao1, L Liu1, J Lu1, Y Lan1, H Wei1, L Xin1, Y Chen1, C Xu1, T Chen1, Y Zhu1, T Jiang5, Z Feng15, W Yang15, Y Wang15, H Zhu16, Y Guan16, G F Gao15, D Li1, J Han1, S Wang1, G Wu1, Y Shu ()1
Date of submission: 28 July 2013
A novel avian influenza A(H7N9) virus causing human infection emerged in February 2013 in China. To elucidate the mechanism of interspecies transmission, we compared the signature amino acids of avian influenza A(H7N9) viruses from human and non-human hosts and analysed the reassortants of 146 influenza A(H7N9) viruses with full genome sequences.
We propose a genetic tuning procedure with continuous amino acid substitutions and reassorting that mediates host adaptation and interspecies transmission.
When the early influenza A(H7N9) virus, containing ancestor haemagglutinin (HA) and neuraminidase (NA) genes similar to A/Shanghai/05 virus, circulated in waterfowl and transmitted to terrestrial poultry, it acquired an NA stalk deletion at amino acid positions 69 to 73. Then, receptor binding preference was tuned to increase the affinity to human-like receptors through HA G186V and Q226L mutations in terrestrial poultry. Additional mammalian adaptations such as PB2 E627K were selected in humans.
The continual reassortation between H7N9 and H9N2 viruses resulted in multiple genotypes for further host adaptation. When we analysed a potential association of mutations and reassortants with clinical outcome, only the PB2 E627K mutation slightly increased the case fatality rate. Genetic tuning may create opportunities for further adaptation of influenza A(H7N9) and its potential to cause a pandemic.
What these researchers did was to collect specimens (as well as clinical and epidemiological information) from human H7N9 cases, along with avian and environmental samples from areas where human cases were identified.
From this they assembled 173 influenza A(H7N9) viruses (103 human and 70 non-human) and analyzed them to try to determine how (and from where) they had evolved.
Remarkably, out of 146 H7N9 viruses with full genome sequences, they detected at least 26 seperate genotypes, mostly from the first wave in 2013. Of those 26, twenty were only detected once or twice, suggesting they were transient, and perhaps not as `biologically fit’ as some of the other genotypes.
Based on their observations, the authors propose that `a genetic tuning procedure with continuous amino acid substitutions and reassortations, mediates the host adaptation and interspecies transmission of H7N9 viruses (Figure 4)’.

Essentially, they describe two processes that they believe facilitate the evolution and adaptation of the virus. Processes that may be `tuning’ the virus in the direction of a `human-adapted’ pathogen.
The first is ongoing reassortment with H9N2 viruses.
Reassortment occurs when two different influenza viruses infect the same host simultaneously. In `close quarters’ they can swap out gene segments, and if they hit the right combination, generate a successful hybrid virus.

Reassortment also produces the biggest, and most abrupt changes in the virus, and is believed the mechanism behind the emergence of many pandemic viruses. You can view a short (3 minute) video from NIAID on reassortment here.
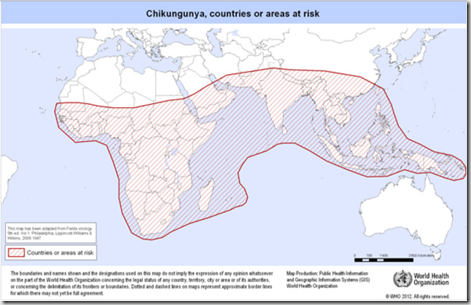
Based on 26 distinct genotypes described in this paper, the reassortment of H7N9 appears to be a vigorous, and ongoing, process. The greatest concentration of genotypes was found in the Yangtze river delta (see map below), suggesting this may be the region where the virus first emerged.

The second evolutionary path occurs as these reassortant viruses passage through different species and pick up specific amino acid changes.
When a virus infects a cell, it immediately sets upon making thousands of copies of itself in order to spread the infection throughout the host. Single-stranded RNA influenza viruses are notoriously sloppy replicators, so invariably, some of these viral copies will carry small transcription errors (in the form of amino acid substitutions).
Most of these `variants’ will prove either neutral or perhaps even detrimental to the survival and propagation of the virus, but occasionally a helpful change occurs (positive selection) that increases the `biological fitness’ of the virus – at least for the current host species.
Viral progeny that are the best suited for their host usually win the replication wars, and soon outnumber and overrun less `fit’ variants. As a result, a better `adapted’ virus can emerge. And if those adaptations help it jump to another host species, it is a viral win-win.
The authors point out that the `mixed bird’ environment of live markets may have helped H7N9’s evolution along, as it was able to spread stealthily, and without interruption, among a variety of species – picking up useful adaptations along the way.
As an example, avian flu viruses bind preferentially to the α2-3 receptor cells found in the gastrointestinal tract of birds. But the H7N9 virus also binds (albeit, not as robustly) to human α2-6 human receptor cells, which are found in mammalian tracheas and upper airways (see Nature: Receptor Binding Of H7N9).
.
The authors speculate H7N9’s partial affinity to α2-6 receptor cells may have been picked up when it passaged through quail or pigeons, which are known to carry both types of cells.
And even once it infects man, the H7N9 virus continues to adapt and evolve, with the PB2 E627K mutation detected in a large number of human isolates. E627K and/or D701N mutations in the PB2 protein are considered critical for mammalian adaptation of avian influenza viruses, as they allow the virus to replicate efficiently in the lower temperatures found in the upper airway.
As H7N9 reassorts and passages through different species – a process the authors call `genetic tuning’ - it continues to evolve, and reinvent itself. Meaning that the virus we get next fall , winter, or spring may not act like the virus we saw during the first two waves.
Obviously, I’ve just covered some of the highlights, and then, only with the broadest of strokes. I’m certain many of my readers will want to read the entire paper. But to close, I’ll let the authors speak to the significance of their findings.
Genetic tuning not only mediated species switching, but may also allow the virus to adapt so that it infects humans more easily and transmits among people more efficiently. Recently, Malaysia reported its first human case of influenza A(H7N9), imported from Guangdong province, China [28]. Rapid transportation and frequent travelling have made it possible to transfer the virus from China to other regions.
Overall, due to the genetic tuning procedure, the potential pandemic risk posed by the novel avian influenza A(H7N9) viruses is greater than that of any other known avian influenza viruses. A response to this threat requires the combined effort of different sectors related to human health, poultry and wild birds, as well as vigilance and co-operation of the world.





![Reassortant pig[6] Reassortant pig[6]](https://blogger.googleusercontent.com/img/b/R29vZ2xl/AVvXsEgppTv7U9dZhh_wVqRdXedk6ElNkgm4B-LSTvmtqAyWYERTknTtfF1FxNLm3GMOlYI6MohfGUmrDBDKSXbAQ22-pDR7LRpCGc9u7IuTcnNUTQVm2hSh0YiTbRFxY5zVhkKqLbG_Ng/?imgmax=800)