@FLA_MEDIC on Twitter
It is hard for me to believe this makes my eighth Thanksgiving blogging at Avian Flu Diary. Somehow, even after 8,000 blog posts, I still find there are new and interesting things to write about nearly every day.
In November of 2006 I began what has turned out to be a joyous tradition for me - taking the time to publicly acknowledge and thank those working in the public health arena to prevent, or mitigate, global health threats, and to mention some of the friends I've made along the way on this remarkable journey through Flublogia.
While I pen AFD alone, this is by no means a solitary effort. I rely (heavily) on the the advice, expertise, hard work, and generosity of dozens of others in Flublogia, without whom, this blog would not be possible.
This is my once-a-year chance to thank them.
You’ll find earlier editions of this roll call at:
Thanksgiving Roll Call 2012
Thanksgiving Roll Call 2011
Thanksgiving Roll Call - 2010
Thanksgiving Roll Call 2009
Thanksgiving Roll Call - 2008
Thanksgiving Roll Call, Redux
AVIAN FLU THANKSGIVING ROLL CALL
Over the years this list has grown in length to the point where it is a bit unwieldy, and so this year I’m trimming it down a bit. This is, in no way, a complete list.
But it’s a start.
You may know some of these people by name, and some by the organizations they represent, while others you may not be aware of at all. So, in no particular order, a tip of the hat and a world of thanks go to:
The career members of the HHS, CDC, and FDA who during the spring of 2009 were faced with an emerging pandemic during a time of political transition. The kind of work they do in the face of an outbreak was nicely dramatized a couple of years ago in the movie Contagion (see The `Contagion’ Conversation Continues).
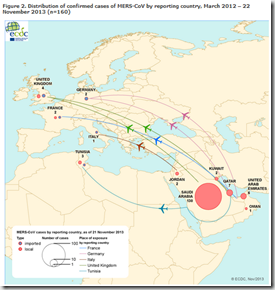
There are countless people at the CDC, the NIH, the WHO, ECDC, FAO, and OIE who are working, mostly anonymously and often in less than optimal conditions, to promote better public health and hopefully to prevent the next pandemic. But four names you might recognize, and may want to follow on twitter are Gregory Hartl and Sari Setiogi at the World Health Organization, Marc Sprenger, director of the ECDC, and Dr. Thomas Frieden, director of the CDC.
There are also researchers and scientists, too numerous to mention, but who’s work moves us closer to understanding infectious diseases. A woefully inadequate list of flu researchers would include:
Dr. Robert G. Webster at St. Jude’s Research Hospital, Greg Poland of the Mayo Clinic, John Oxford, Professor of Virology at St Bartholomew’s and the Royal London Hospital, Dr. Allison E. Aiello at the University of Michigan, Professor Peter Doherty, and Richard Webby of St. Judes, Ab Osterhaus and Ron Fouchier of Erasmus Medical Center in Rotterdam, and Chairul A. Nidom, at the Tropical Disease Centre at Airlangga University.
And there are universities and medical centers around the world; places like the University of Minnesota, St. Jude Research Hospital, UPMC Center For Biosecurity,The University of South Florida, Australian National University, and Baylor College of Medicine in Houston, which are major sponsors of influenza and emerging infectious disease research - along with others too numerous to mention.
Readers of this blog no doubt have noticed that I’ve referenced the work of CIDRAP often over the years. The reason is simple: The reporting from CIDRAP News is always first rate, with most of the heavy lifting done by Editor Robert Roos, and Lisa Schnirring.
Besides, Dr. Michael Osterholm, Director of CIDRAP, is arguably the best spokesperson on pandemic influenza in the country. Before devoting his attentions to CIDRAP, Dr. Osterholm served for 24 years (1975-1999) in various roles at the Minnesota Department of Health (MDH), the last 15 as state epidemiologist and chief of the Acute Disease Epidemiology Section.
I consider myself fortunate indeed to have become friends with Lisa, Robert, Nick Kelley – CIDRAPs Preparedness Program Coordinator - and Dr. Osterholm.
All of them have been very supportive of me, and my blog, and I am very grateful.
CIDRAP, of course, is made up of more than just the handful of people I've mentioned. A more complete list is available here along with their mission statement.
This year I’m extraordinarily pleased to help welcome Virologist Dr. Ian Mackay, curator of the Virology Down Under Blog, and associate professor of clinical virology at the University of Queensland to Flublogia.
Not only does Ian lend a much appreciated level of scientific expertise to the flu blogging scene, he’s fun to read, and a genuinely nice fellow. If you aren’t already reading his blog, you need to add him to your list.
Last year I added a new friend, Dr. John Sinnott, MD FACP FIDSA and Director of the Florida Infectious Disease Institute, who has also been extraordinarily kind to this blogger.
I’d be remiss if I didn’t mention another generous MD, Dr. Michael Greger, Director of Public Health and Animal Agriculture at the Humane Society of the United States, and author of Bird Flu: A Virus of Our Own Hatching. The entire text of which is available online, without charge (thank you Dr. Greger!).
Among members of the fourth estate, there are some truly remarkable science and health writers and reporters.
Helen Branswell, health reporter for the Canadian Press, has produced some of the finest reportage on the emergence of the H5N1 virus (and now H1N1) as exists anywhere in the world, and she started back when few had heard of the threat.
Her writing is clear, concise, and absent of the breathless prose that many lesser journalists rely upon. Whenever I find a Branswell article, I know in advance it is going to be well worth reading.
Likewise, Maggie Fox - who has recently moved over to NBC News from the National Journal (and before that, Reuters) - is another standout in the world of health reporting. Maggie understands the science, having completed fellowships at the National Institutes of Health on Genomics, at Harvard Medical School on infectious disease, and at the University of Maryland on child and family health policy.
Declan Butler, senior reporter for Nature, and blogger, who very early on called the attention of the world to the pandemic threat, and who has used Google Earth to great effect mapping avian flu outbreaks around the world.
And for overall excellence in science writing I would also hasten to mention Carl Zimmer at The Loom and Ed Yong at Not Exactly Rocket Science, both of whom relocated to National Geographic over the past year.
Other luminaries in the health & science field include Jason Gale of Bloomberg, Patrick Thibodeau of ComputerWorld, Betsy McKay at the Wall Street Journal, Robert Bazell at NBC News and Dr. Richard Besser at ABC News, and Laurie Garrett at Foreign Policy.
On the Internet we have a number of dedicated and astute bloggers, and they too deserve special mention. Among them:
Crawford Kilian, author of Crofsblog, was one of the first to devote his blog to pandemic flu – but has branched out to cover many of the neglected diseases and disasters - like Dengue, Malaria, Chikungunya, and the Cholera epidemic in Haiti.
Writer and blogger Maryn McKenna lends considerable talent and expertise to Flublogia, particularly on the antimicrobial resistance front.
In 2010 her second book, SUPERBUG: The Fatal Menace of MRSA was published to sterling reviews (you can read my review here). Her Superbug Blog continues to be one the best resources on antibiotic resistance issues available online. Maryn is also the author of Beating Back The Devil, the inside story of the CDC’s Epidemic Intelligence Service, and an upcoming book on MRSA.
Ian York, who now works at the CDC, also pens the wonderful Mystery Rays blog (although his work schedule has severely limited his blogging). His eclectic meanderings through the world (and history) of infectious diseases are a delight for disease geeks and highly recommended.
In 2009, after several years of email correspondence, I finally got to meet the irrepressible (and now zombified!) Scott McPherson. We were both part of the CIDRAP H1N1 summit in September 2009, and I got to spend two glorious days hanging out with him and Indigo Girl (of the AllNurses forum), forming what we called The Flu Amigos.
A fellow Floridian, Scott is the CIO of the Florida House of Representatives, and rubs elbows with State and Federal officials every day. His insights, often sprinkled with a dash of healthy whimsy, are always a pleasure to read. I remain hopeful that Scott will resume blogging on a regular basis again in the future.
While not necessarily flu-centric, some other bloggers of note that I follow, and recommend include:
Vincent Racaniello’s always excellent Virology Blog, which devotes a good deal of time to influenza. His TWiV and TWiP podcasts are also highly recommended.
Assistant Professor of Epidemiology, Tara Smith’s blog Aetiology and Celeste Monforton and Liz Borkowski of The Pump Handle are highly recommended as well.
Jim Garrow’s The Face of the Matter explores emergency communications in an age of social media.
And for a variety of infectious disease news, there’s Giuseppe Michieli’s eclectic A Time’s Memory.
And last, but hardly least, there’s Dr. Peter Sandman who, along with his wife and colleague Dr. Jody Lanard, produce a wealth of invaluable risk management and pandemic communications advice on their Risk Communication Website.
Relatively new are the Twitter generated daily newspapers, like Cesar Sanchez’s Microbiology Daily, and All Hands’s Emergency Management Daily and Business Continuity Daily, Jim Garrow’s Public Health Daily, and Dave Walker’s Healthcare Daily.
In a special category I mention author, journalist, filmmaker, and friend Peter Christian Hall who’s pandemic novel American Fever (see It Gives You Fever ) was published in paperback this year. After the release of the movie `Contagion’ - Peter interviewed flu bloggers for The Huffington Post (see Contagion Grips ‘Flublogia').
And every day outside of the limelight dozens of hardworking flubies scour foreign language news reports, using search engines, text-finding software, and translating programs to bring us the latest tidbits of news from around the world.
While there are many who contribute, some of the names that pop up most often on the sites I visit include: Gert van der Hoek, Shiloh, Pathfinder, Emily, Sally, Giuseppe Michieli, Treyfish, Commonground, Carol@SC, mojo, bgw in MT, Readymom, Sharon Sanders, Cottontop, dbg, Tetano, Diane Morin, Missouriwatcher, and Ronan Kelly.
There are many others, of course. My sincere apologies to those I failed to name.
I’ve written numerous times about the work they do, but if you want to know how they do it, check out Newshounds: They Cover The Pandemic Front. The work they do is remarkable. And I couldn't do much of what I do without them. Thank you all.
The owners and moderators of the flu forums deserve mention, too.
Labors of love, and devourer's of both time and money, flu forums provide a place for laymen and professionals to gather to discuss the various aspects of pandemic planning, and quite often, the science behind influenza and epidemiology. The founders and moderators do a terrific job keeping things on track, and do so without compensation. Most of the time, the costs (which can run into the hundreds of dollars each month) are borne by the owners.
There are a number of flu forums out there, but the two where I hang my hat are the Flu Wiki and Flutrackers. Each has their own style and personality, and in many cases, members of one forum belong to several other forums as well. The Flu Wiki, the first of the dedicated flu forums, was founded by DemFromCt, Pogge, and Melanie Matson. In 2008, we lost Melanie after a long illness. She was a pioneer, and an activist, and is greatly missed.
FluTrackers, founded by Sharon Sanders (but is run with the aid of dozens of tireless volunteer moderators), boasts nearly 2,000 members and prides themselves on maintaining an impressive library of scientific literature on pandemic influenza and other emerging infectious diseases.
Sharon is also a dear friend, fellow Floridian, confidant, and unindicted co-conspirator.
And then there are the flubies, which number in the thousands. Some are active posters on the flu forums, while others take a more passive role. Many have become activists in their communities.
Readymom, whom I've highlighted before in these pages, runs her own website Emergency Home Preparation.
Starting in mid-2007, more than a dozen volunteers worked to put together the GetPandemicReady.Org website. There you will find more than 3 dozen easy-to-follow preparedness guides, written by some pretty familiar names from the Flu Forums.
Now is a good time to remind my readers that agencies like the Red Cross, Red Crescent, CARE, Save The Children, UNICEF, and others are working around the world every day to combat poverty and disease, including pandemic flu.
They could use your support. These NGO’s do a great deal with very little, and even small donations can help make a difference.
Often forgotten, I also send out thanks to all who wear the uniform of our country, and who will are often called upon to be on the front lines during any crisis, including a pandemic.
This includes our military and national guard troops, both at home and abroad. You guys and gals do a tough, often thankless job, 365 days a year; and are deserving of both our respect and our nation's gratitude.
Please know, you have mine.
There are hundreds of thousands of doctors, nurses, technicians, EMT's, paramedics, firefighters, and law enforcement officers out there who put it on the line each and every day. I'm proud to have been able to be a part of that universe. And my thanks, and fervent best wishes go out to each of you.
And of course, thanks go to the readers of these forums and blogs. There are far more of you out there than you imagine.
Those that post on flu forums, or comment on blog sites are just the tip of the iceberg. Ninety percent of our visitors read and absorb the information here, and say nothing. We know you are out there because our web counter software logs every visit.
No, I’m not going to `out' anyone. Your secret is safe with me.
But even this humble blog gets visits every day from hundreds of corporations, government agencies, financial institutions, and even medical research facilities. Names that you would readily recognize. And that is both extremely gratifying and humbling at the same time.
It has been an amazing journey, these past eight years blogging on influenza and emerging infectious diseases. I've been fortunate enough to meet scores of people, either in person, or via email or chat, from around the world due to this blog.
To Camille, Sharon & Lance, Cliff, Cheryl, Scott and Crof, Maryn, Maggie and Helen, MTO & Lisa & Nick & Robert at CIDRAP, Chacal & Family, Dr. John Sinnott, Dr. Ian Mackay, Jody Lanard & Peter Sandman, Peter C. Hall, Anne, Eric Starbuck, Rolf, Dr. Michael Greger, Jim in Thailand, Anne, Seazar, Paul, Joel, AnnieRn, Caroldn,and Bonnie (and many more I've no doubt left out) a special holiday thanks to you and your families.
You guys, whether you know it or not, help light the path for me every day.
And to everyone else, a safe, happy, and healthy Holiday.
Editor’s Note; I’m having two wisdom teeth extracted later today (and at my age!) , and so I probably won’t be blogging anymore today and probably not tomorrow as well.
Given how loopy pain pills make me, that’s probably a good thing. ;)