Credit TFAH
# 8171
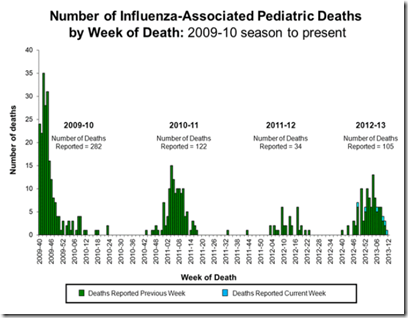
After a couple of fairly tame influenza seasons that followed the 2009 H1N1 pandemic, last year saw a particularly nasty H3N2 season - affecting mostly elderly patients - that produced some of the highest hospitalization and P&I mortality rates that we’d seen in a decade (see CDC Statement On Elevated P&I Mortality Rate).
While the uptake of seasonal flu vaccines have improved in recent years among those over the age of 65, and for children aged 6mos to 17 years, most young adults (aged 18-65) in the United States still elect not to get the vaccine.
The irony here is, while most years the flu shot provides a moderate level (50%-60%) of effectiveness, the age cohorts most likely to enjoy the best protection are those same younger adults who tend to eschew the jab.
This year, we are seeing the pH1N1 strain dominate for the first time since 2010, and as it did in 2009, it appears to be hitting those same younger adults harder than usual. Today, TFAH (the Trust for America’s Health) released a report on the uptake of the flu vaccine from the 2012-2013 flu season, that illustrates these trends.
Issue Brief: As Flu Season Ramps Up, Adults 18-64 Years Old Least Likely to Get Flu Shots
January 2014
Analysis Finds 32 States Fail to Vaccinate at least 40 Percent of Adults 18-64 Years Old
An analysis by the Trust for America’s Health (TFAH) found that only 35.7 percent of adults ages 18 to 64 years old got the flu shot last season (the most recent period data with available data). By comparison, 56.6 percent of children (ages 6 months to 17 years old) and 66.2 percent of seniors (ages 65 and older) were vaccinated. The U.S. Centers for Disease Control and Prevention (CDC) recommends all American 6 months and older get vaccinated each year.
According to the CDC, the flu season in the United States is beginning to “ramp” up and flu is now widespread in 35 states. Rates are particularly high in 13 Southern and Central/Western states (Alabama, Arkansas, Indiana, Kansas, Louisiana, Mississippi, Missouri, Nevada, New Mexico, North Carolina, Oklahoma, Texas and Utah).
H1N1 is the most prevalent flu strain this season, which can disproportionately and adversely impact otherwise healthy children and young adults, according to the CDC.
“The trend of low vaccination rates among younger adults is particularly troubling this year, when they are more at risk than usual for the effects of the H1N1 strain of flu that’s circulating,” said Jeffrey Levi, PhD, executive director of TFAH.
Today’s analysis finds that overall flu vaccination rates remain low in the United States. Fewer than half of Americans (45 percent) got a flu shot during the 2012-13 season, which was an increase over 41.8 percent in the previous (2011-12) season.
Whether it is due to complacency, a feeling of invulnerability, or a general distrust of vaccines or big Pharma, getting the seasonal flu shot remains a low priority for many young adults.
Knowing this, vaccine manufacturers only produce as much vaccine as they think are likely to be sold each year, else millions of shots would go wasted.
This year, as we see from the CDC’s Vaccine Distribution chart below, for the United State’s population of over 300 million people only about 140 million shots were ordered.
Seasonal Influenza Vaccine & Total Doses Distributed
- This table reflects the cumulative weekly total number of seasonal influenza vaccine doses distributed in the US as reported to CDC by influenza vaccine manufacturers and selected distributors.
- Currently, manufacturers project 138-145 million doses of flu vaccine to be produced this season.
January 9, 2014 2:00 PM ET
Table of 2013-14 Seasonal Influenza Vaccine—Total Doses Distributed
In a related story , Helen Branswell wrote last night about the flu shot shortage in Canada – brought on by the recent climb in serious flu infections among young adults.
The flu shot shortage: Who’s to blame?
By Helen Branswell Medical reporter, The Canadian Press
Wonder why some Canadians have to scramble to find a flu shot this year? People may be tempted to blame the authorities – their provincial or territorial government – but to do so would be unfair.
If people are looking for a culprit for this year’s flu shot shortage, they should probably stand in front of a mirror.
It’s as simple as this: Canada doesn’t have more vaccine because it hasn’t used more vaccine in the past.
There is actually another, potentially dangerous, downside to the low demand for seasonal flu shots.
Just as vaccine manufacturers can’t afford to produce enough vaccine for everyone in the United States and Canada, knowing that more than half of the doses would be discarded, they also can’t afford to build and maintain enough manufacturing capacity to quickly produce sufficient pandemic vaccine for the global population quickly.
If the demand for yearly vaccines were considerably greater, the industry would build the infrastructure needed to produce it, and as a result their capacity to produce vaccines during an emergency would increase as well.
For now, the ability of vaccine manufacturers to quickly produce and deliver large quantities of pandemic influenza vaccine remains very limited. Some vaccine would likely be available within 6 months – but not the kind of quantities that would be required to stop a pandemic in its tracks.
The limits of our current vaccine manufacturing technology, and the steps needed to improve them, are many and complicated, and go far beyond the need to increase yearly uptake of vaccines. They were were well addressed back in the 2012 in CIDRAP: The Need For `Game Changing’ Flu Vaccines – a truly impressive 160-page report that emphasizes the need for a revolution in vaccine technology.
The Compelling Need for Game-Changing Influenza Vaccines
An Analysis of the Influenza Vaccine Enterprise and Recommendations for the Future
Michael T. Osterholm, PhD, MPH, Nicholas S. Kelley, PhD, Jill M. Manske, PhD, MPH, Katie S. Ballering, PhD, Tabitha R. Leighton, MPH, Kristine A. Moore, MD, MPH
For those not ready to commit to reading a 160-page report, there is a 12-page Executive summary available.