Note: I don’t usually write about family or personal events in this blog, but today I hope you’ll forgive me if I make an exception.
# 6174
In a couple of hours I’ll be making a 50 mile drive to see my Dad, possibly for the last time. He is 87, in failing health, and (thankfully) receiving almost daily home hospice care.
Dad, who hates the idea of being in the hospital, has stated his last goal is to die in his own bed. Something that my sister and I are trying to make happen.
To that end, we’ve prepared for this day for well over a year. In fact, I discussed some of our pre-planning a year ago in On Having `The Conversation’, a brief excerpt from which follows:
We’ve discussed, in detail, exactly what Dad would want us to do if he were unable to make medical decisions for himself.
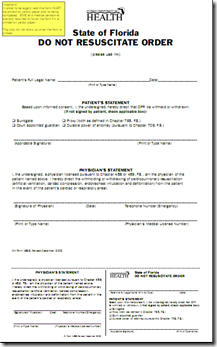
In fact, a few months ago Dad asked if I would get for him a legally binding Do Not Resuscitate (DNR) order, so that if something happened to him, and an ambulance were called, no heroics would be performed.
Verbal instructions by family members – even if the patient is in the last stages of an incurable illness – are likely to be ignored by emergency personnel.
Dad now proudly has the bright yellow DNR order posted over his bed, and carries another credit-card sized one in his wallet.
In Florida, the form must be printed on yellow paper. Different states have different requirements. You should check with your doctor, or the local department of health to determine what the law is in your location.
We’ve also had (for many years) a living will and a Health Care Proxy drawn up for Dad, so either my sister or I can make decisions regarding Dad’s health care should he no longer be able to.
Sensing his time was growing short last fall, Dad insisted on going down to the local funeral home to make his own prepaid funeral arrangements.
He didn’t want anyone else to have to make those decisions when the time came.
When his health really began to decline over the Christmas holiday, we discussed several matters, including bringing in home hospice care.
Dad, who has always been fiercely independent, balked at first, but it soon became apparent to him that my sister could no longer physically provide all of the care he would need.
Although they’ve been coming only for a few weeks, the hospice nurses and doctor have done a great deal to relieve Dad’s pain, to make him more comfortable, and relieve my sister of some of her care giving duties.
Having home healthcare visits mean he no longer must make the monumental efforts to bathe, dress, and be driven by my sister to see his doctor.
In other words, it’s been an absolute Godsend.
In retrospect, I wish we’d have brought them in a little earlier, but I doubt that until after Christmas, Dad would have agreed.
The end appears to be coming quickly now.
His nurse believes his kidneys are failing and he’s in and out of consciousness a lot. The morphine, which at long last is controlling his intractable pain, blurs reality for him as well. Lucid moments are becoming rarer.
When awake he’s mostly `travelling’ now; talking to friends long departed, revisiting the adventures of his youth (he was in the Navy in WWII, and a private pilot in civilian life), and earlier this week proudly announced he’d been hired to build one last skyscraper in Tampa.
Not a bad thing, considering. He’s not afraid, and he’s not in pain. I’ll settle for that.
Over the past dozen years my sister and I have seen Dad through 3 cancer surgeries, two major eye operations, Mom’s passing 6 years ago, a car wreck followed by 5 weeks in rehab, and a couple other health crises.
It isn’t easy to accept that we’ve done what we can, that we’ve reached the end of a long road, and now it’s time to day goodbye.
But that’s where things stand. And while you can hate it, there’s no changing it.
The fact that we’ve taken the steps to ensure that Dad gets to go out of this world on his own terms - at peace, without being poked and prodded, and in his own bed - help immensely. It was literally his last wish.
That, and his hope that we not make a big fuss over his passing. “It’s time,” he said when we last spoke, “and I’ve had a damned good ride.”
I talk about preparedness a lot in this blog.
Most of the time, it is on preparing to survive a disaster or some kind of emergency, but there are other types of preparedness as well. And preparing for the end that must come to each of us, is one of them.
As a medic, I’ve seen the anguish that relatives suffer when trying to make life or death decisions on behalf of a loved one.
These are deeply emotional issues, and can create life-long rifts in the fabric of families.
While nothing can eliminate the emotional trauma that comes with a medical crisis or the impending loss of a loved one, making rational decisions in advance – and making them known and binding – can greatly reduce the strain later.
While I know it hasn’t always been pleasant or easy for Dad to consider the practicalities of his final days, I think he considers that to be his parting gift to my sister and myself.
Something that, I can assure you, both of us appreciate.