# 4773
With the recent attention being paid to Dengue and other vector borne diseases here in Florida and around the United States, public health departments are urging people to become more diligent about removing breeding places for mosquitoes around their homes.
But it isn’t just outside the home where people need to check . . . some mosquito species are perfectly capable of setting up light housekeeping inside the home as well.
While the Aedes aegypti is most commonly associated with spreading disease, the Aedes Albopictus or `Asian tiger’ mosquito is quite capable of doing so as well.
A couple of resources and some discussion.
First, a link to the South Florida Sun Sentinel which has a story about one type of Dengue mosquito found breeding inside south Florida residences.
Mosquitoes carrying dengue fever can live indoors
Aedes has been found in Waterpiks, fridge trays, toilets
By Bob LaMendola, Sun Sentinel
7:43 PM EDT, July 30, 2010
Next, a timely study which appears in PLoS One titled:
Indoor-Breeding of Aedes albopictus in Northern Peninsular Malaysia and Its Potential Epidemiological Implications
Hamady Dieng1*, Rahman G. M. Saifur1, Ahmad Abu Hassan1, M. R. Che Salmah1, Michael Boots2, Tomomitsu Satho3, Zairi Jaal1, Sazaly AbuBakar4
Background
The mosquito Ae. albopictus is usually adapted to the peri-domestic environment and typically breeds outdoors. However, we observed its larvae in most containers within homes in northern peninsular Malaysia. To anticipate the epidemiological implications of this indoor-breeding, we assessed some fitness traits affecting vectorial capacity during colonization process. Specifically, we examined whether Ae. albopictus exhibits increased survival, gonotrophic activity and fecundity due to the potential increase in blood feeding opportunities.
Methodology/Principal Findings
In a series of experiments involving outdoors and indoors breeding populations, we found that Ae. albopictus lives longer in the indoor environment. We also observed increased nighttime biting activity and lifetime fecundity in indoor/domestic adapted females, although they were similar to recently colonized females in body size.
Conclusion/Significance
Taken together these data suggest that accommodation of Ae. albopictus to indoor/domestic environment may increase its lifespan, blood feeding success, nuisance and thus vectorial capacity (both in terms of increased vector-host contacts and vector population density). These changes in the breeding behavior of Ae. albopictus, a potential vector of several human pathogens including dengue viruses, require special attention.
Although this particular study is set in Malaysia, the Aedes albopictus mosquito has made extensive inroads in the rest of the world over the past 40 years, and is considered one of the top 100 worst invasive species according to the Global Invasive Species Database.
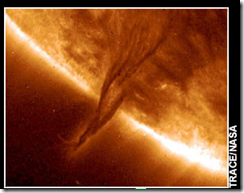
Dark Blue indicates the A. Albopictus native range, while green indicates new introductions in last 40 years.
While mosquitoes are pretty much ubiquitous here in Florida, as well as in and many other areas, one shouldn’t panic over being bitten.
The vast majority of mosquitoes here in the US are not carrying infectious diseases.
The odds of contracting West Nile Virus, Dengue, EEE, or any of the mosquito borne encephalitis viruses are actually pretty small.
In order to vector a disease, they first must bite a host(bird, animal, or human) that is viremic – infected and with sufficient viral material in their bloodstream.
Still, it makes sense to take precautions.
Like wearing DEET when you are outdoors, wearing long sleeves and pants, and removing breeding places inside and outside of your home.
Any container of water . . . even as small as a bottle cap . . . can breed mosquitoes. Containers with houseplants appear to be particularly good homes for these pests.
For more details visit the Florida DOH Mosquito-borne Disease Prevention webpage.