Photo Credit- Wikipedia
# 9995
You may recall that just two weeks ago, HK authorities reported their first Wild Bird Found Infected With H5N6 – a peregrine falcon – and over the past decade they’ve seen scores of (mostly migratory) birds carrying the H5N1 virus. Hong Kong is one of the few places in the world where public health authorities take notice of something as seemingly inconsequential as a single dead bird.
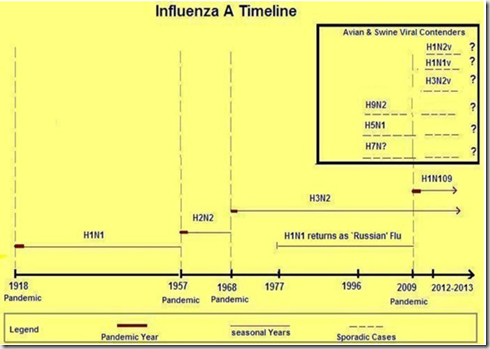
To understand why, you have to go back to 1997, when the H5N1 Bird Flu virus suddenly appeared in Hong Kong – infecting 18 residents and killing 6. The source of the infection turned out to be their own domesticated poultry industry, likely infected by wild birds.
It was only the complete eradication of all poultry in the territory that managed to halt what many feared could have been a disaster. Since then, Hong Kong has kept a particularly watchful eye on their winged visitors.
The strain of HPAI H5 in today’s case has yet to be determined, but authorities are already advising poultry interests of the potential threat.
This from Hong Kong’s CHP.
Oriental magpie robin tests positive for H5 virus
Preliminary testing of an Oriental magpie robin found in Sai Kung has returned a positive result for the H5 avian influenza virus, a spokesman for the Agriculture, Fisheries and Conservation Department (AFCD) said today (April 30), adding that further confirmatory tests are being conducted.
The sick Oriental magpie robin was found and collected near 10B Sha Kok Mei First Lane, Sai Kung yesterday (April 29). Oriental magpie robins are common resident birds in Hong Kong.
The spokesman said cleansing and disinfection have been stepped up at the venue, adding that there are no poultry farms within three kilometres of where the dead bird was found.In view of the case, the AFCD has phoned poultry farmers to remind them to strengthen precautionary and biosecurity measures against avian influenza. Letters have been issued to farmers, pet bird shop owners and licence holders of pet poultry and racing pigeons reminding them that proper precautions must be taken.
The spokesman said the department would conduct frequent inspections of poultry farms and the wholesale market to ensure that proper precautions against avian influenza have been implemented. The department will continue its wild bird monitoring and surveillance.
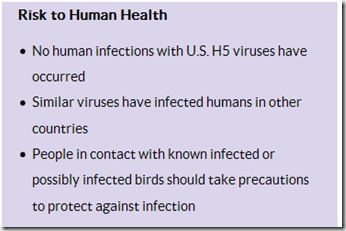
"People should avoid personal contact with wild birds and live poultry and their droppings. They should clean their hands thoroughly after coming into contact with them. The public can call 1823 for follow-up if they come across suspicious, sick or dead birds, including the carcasses of wild birds and poultry," the spokesman said.
The Food and Environmental Hygiene Department (FEHD) will continue to be vigilant over imported live poultry as well as live poultry stalls. It will also remind stall operators to maintain good hygiene.
The Department of Health will keep up with its health education to remind the public to maintain strict personal and environmental hygiene to prevent avian influenza.
The AFCD, the FEHD, the Customs and Excise Department and the Police will strive to deter the illegal import of poultry and birds into Hong Kong to minimise the risk of avian influenza outbreaks caused by imported poultry and birds that have not gone through inspection and quarantine.
All relevant government departments will continue to be highly vigilant and strictly enforce preventive measures against avian influenza. Health advice is available from the "H5N1 Health Advice" page on the AFCD website at www.afcd.gov.hk.Ends/Thursday, April 30, 2015
Issued at HKT 20:44
NNNN