Credit World Health Organization – May 2003
# 6964
This third week of February, the 21st day to be exact, is the 10th anniversary of the arrival of SARS (Severe Acute Respiratory Syndrome) to Hong Kong. While the virus had been percolating stealthily across rural China since the previous November, this was its first known border crossing.
The virus arrived via a 64-year-old Chinese physician from neighboring Guangdong Province who had recently treated atypical pneumonia cases at Zhongshan hospital.
Asymptomatic when he began his journey, by the time he checked into a 9th floor room of the Metropole Hotel, he was beginning to show signs of illness. Exactly how the virus was transmitted to a dozen guests or more staying at that four-star hotel may never be known.
Perhaps he coughed while standing in a crowded elevator, or contaminated door handles or the pen at the register when he signed in at the lobby. It was speculated he might have even vomited in the hallway.
In October of 2003, WHO issued a consensus document on the epidemiology of SARS that included:
– The implications of the Metropole Hotel outbreak are not yet fully understood.
Intensive investigations of circumstances surrounding the late-February outbreak in the Metropole Hotel, Hong Kong, which seeded the international spread of SARS, have not yet answered all questions. During this incident, the virus was transmitted to at least 16 guests and visitors, all linked to the 9th floor of the hotel. The results of environmental sampling on the carpet outside room 911, where the index case resided, and elevator areas show a hot zone (possibly vomitus or respiratory secretions). Samples were PCR positive for the virus 3 months after the index case spent a single night at the hotel. Although tests demonstrated the presence of SARS coronavirus RNA and not viable virus, this finding may have implications for the persistence of the virus in the environment.
The Metropole Hotel outbreak is recognized as a “superspreading event”. However, the index case did not have an unusually high viral load when tested on days 9 and 11 of illness.
By whatever means, Dr. Liu Jianlun – who died in a Hong Kong hospital two days later – became known as as the first international `super spreader’ of the disease.
The results of his fateful visit to Hong Kong are recounted below in the WHO document Severe acute respiratory syndrome (SARS): Status of the outbreak and lessons for the immediate future.
Days later, guests and visitors to the hotel’s ninth floor had seeded outbreaks of cases in the hospital systems of Hong Kong, Viet Nam, and Singapore.
Simultaneously, the disease began spreading around the world along international air travel routes as guests at the hotel flew home to Toronto and elsewhere, and as other medical doctors who had treated the earliest cases in Viet Nam and Singapore travelled internationally for medical or other reasons.
This still unidentified virus quickly began to show up in Vietnam, Singapore, and even Toronto – and hospital workers – unaware that a new, virulent and highly infectious pneumonia virus was before them, were exposed and infected.
By March 12th, after reviewing the situation in Hanoi, Hong Kong, and Beijing, WHO issues a global alert about cases of atypical pneumonia warning that Cases Of Severe Respiratory Illness May Spread To Hospital Staff.
Two days later (March 14th), three cases appeared in Singapore, brought in most likely by a flight attendant who had also stayed at the Metropole hotel in Hong Kong.
The next day, the World Health Organization issues emergency travel advisory as it became apparent that whatever this virus was, it was spreading rapidly.
This syndrome, SARS, is now a worldwide health threat,” said Dr. Gro Harlem Brundtland, Director General of the World Health Organization. “The world needs to work together to find its cause, cure the sick, and stop its spread.”
While the virus was definitely on the move, eventually making it to more than 30 countries, no city was harder hit than was Hong Kong.
Between March 11th and June 6th, a total of 1750 cases were identified, and of those, 286 died.
In time, the virus was identified, and contained (see Hong Kong’s Coronavirus Response), with quarantine being the most effective weapon in the public health department’s arsenal.
But not before nearly 8,000 were infected worldwide, and nearly 800 died.
Bad . . . but not as bad as it might have been. In many ways we were lucky that time.
Unlike with influenza, patients were not infectious until they displayed overt symptoms, making the identification and isolation of cases possible.
Last month, In EID Journal: A Brief History Of Quarantine, we looked at the long, successful history of this most basic of public health interventions, and how it was utilized during the SARS outbreak. I wrote:
During the 2003 SARS epidemic, Isolation was used in the United States for patients who were ill, but since transmission of the virus was very limited here, quarantine was not recommended for those exposed (cite).
In other countries, where transmission risks were greater, quarantines were used – quite successfully – in order to contain the virus.
- Singapore was one of the first countries to mandate quarantines when more than 800 family members of SARS patients were ordered to stay in their homes.
- Hong Kong sealed part of the Amoy Gardens Apartment complex after scores of cases erupted there, and later moved all remaining residents to two holiday camps where they were quarantined.
- And Toronto, Canada closed schools and quarantined thousands in their bid to contain the virus (see The SARS Experience In Ontario, Canada).
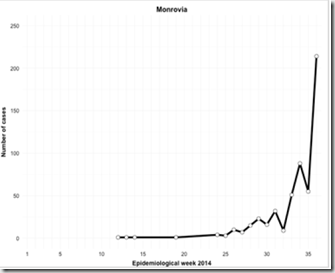
The graph below shows two distinct phases of disease transmission in Canada, both apparently dampened by the implementation of quarantines.

While the aggressiveness of quarantine measures taken in Toronto have been criticized by some (see Severe acute respiratory syndrome: Did quarantine help?), many experts have stated that quarantining those exposed (usually in their own homes) helped to halt the epidemic.
The full story of the SARS outbreak is both long, and fascinating, and I heartily recommend both Karl Taro Greenfeld’s The China Syndrome: The True Story of the 21st Century's First Great Epidemic and David Quammen’s excellent book Spillover: Animal Infections and the Next Human Pandemic.
The remembrance of this crisis has no doubt helped to amplify the concerns of the public - and health officials - in Asia, and around the world over the recent emergence of another coronavirus in the Middle East.
This novel coronavirus (NCoV) is not SARS, and so far it has failed to demonstrate an ability to spread as easily as did SARS.
Nevertheless, this week - along with a lot of media stories recalling the the 2003 SARS epidemic, we are seeing a number of cautionary statements from doctors and researchers regarding this NCoV.
Vigilance urged over new coronavirus
Concerted efforts in enhancing surveillance and control measures for novel coronavirus
Not because they are convinced that this newest coronavirus presents an immediate or inevitable public health threat. But because the remarkable success in containing the 2003 SARS epidemic demonstrated the value of a swift, and coordinated, global public health response.
The future of NCoV is highly uncertain right now. It could continue to threaten - or it could easily fizzle – finding itself unable to adapt well enough to humans to thrive.
These are, as they say, early days.
But if NCoV does fade away, it might very well be due to the unsung efforts of local, regional, and global health officials and researchers (at the WHO, ECDC, CDC, CHP, HPA, etc) who are currently seeking to better understand this virus, and contain its spread.
The old saying is true, `When public health works, nothing happens’.