# 8989
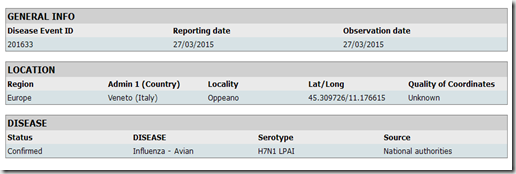
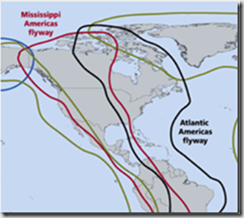
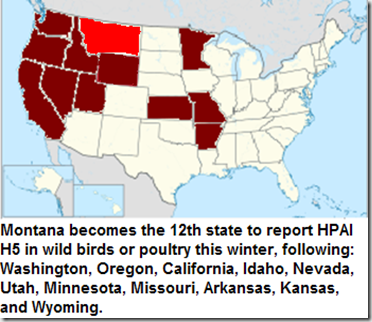
Although I’ve not yet found an official source, The Missoulian is reporting that a captive gyrfalcon in Columbia Falls (Northwest Montana, very near the Canadian border) has died from HPAI H5N2 after being fed a wild duck. Montana becomes the 12th state to report the detection of HPAI H5 this winter.
The bird that died was owned by a falconer who owns roughly 50 other birds, all of which will be tested for the virus.
First a brief excerpt from a much longer report, then I’ll be back with a bit more:
Poultry producers warned as bird flu kills captive falcon in Columbia Falls
By Vince Devlin
COLUMBIA FALLS – The death of a captive gyrfalcon here was caused by highly pathogenic avian influenza, the Montana Department of Livestock confirmed Tuesday.
It’s the first case, outside of hunter-harvested wildlife, reported in Montana in years.
The influenza can decimate commercial poultry stocks, killing up to 99 percent in an infected flock.
No mortalities in domestic poultry in the state due to avian influenza have been detected, and no human health issues have been reported for this particular strain, H5N2, to date.
Martin Zaluski, a veterinarian with the Department of Livestock, said the avian influenza is primarily found in wild waterfowl.
“However, the extent of avian influenza in the Continental flyways right now is unprecedented,” Zaluski said, and infected domestic poultry has been found in several states in the past several weeks, including Idaho, Washington and Oregon.
The rate of spread of these HPAI H5 viruses across the western states has been truly remarkable, and it is expected that additional states will be added to the list in the weeks and months to come.
While primarily a concern for the poultry industry, a week ago, in CDC: HPAI H5 Viruses In The United States, we looked at the CDC’s advice regarding these avian viruses.
Meanwhile, the USDA offers the following biosecurity advice for those who may come in contact with wild birds:
Bird Enthusiasts:
Do not pick up deceased or obviously sick birds. Contact your State, tribal, or Federal natural resources agency if you find sick or dead birds.
- Wear rubber gloves when cleaning your bird feeders.
- Wash hands with soap and water immediately after cleaning feeders.
- Do not eat, drink, or smoke while cleaning bird feeders.
Hunters:
Follow routine precautions when handling wild birds.
- Do not handle or consume game animals that are obviously sick or found dead.
- Do not eat, drink, or smoke while cleaning game.
- Wear rubber gloves when cleaning game.
- Wash hands with soap and water, or alcohol wipes, immediately after handling game.
- Wash tools and working surfaces with soap and water and then disinfect.
- Keep uncooked game in a separate container, away from cooked or ready-to-eat foods.
- Cook game meat thoroughly; poultry should reach an internal temperature of 165 degree Fahrenheit to kill disease organisms and parasites.
- To report unusual signs in birds you have seen in the wild, call 1-866-4-USDA-WS. To learn more about how you can help, visit usda.gov/birdflu.