Salmonella typhimurium bacteria – Credit CDC PHIL
# 6599
You might not think there’d be much of a connection between an emergent serotype of Salmonella and the HIV epidemic in Sub-Saharan Africa - but if researchers from the Wellcome Trust Sanger Institute have it right - this highly pathogenic bacterial strain may have had a powerful viral ally.
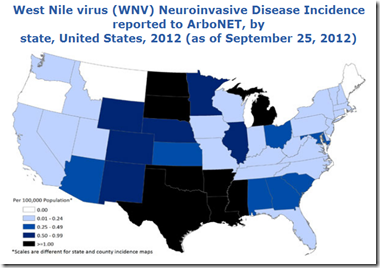
There are more than 2500 serovars of Non-Typhoidal Salmonella (NTS) that can produce gastroenteritis or other infections in humans. Taken together, these Gram negative, anaerobic bacteria are believed to be the second most common source of food poisoning in the United States.
Those infected often develop diarrhea, fever, vomiting, and abdominal cramps that may persist for several days.
In the western world most recover without treatment, although the CDC estimates that nearly 400 people infected die each year in the United States (Cite CDC Food borne Illness Estimates).
In developing countries, Non-typhoidal Salmonella can (and does) exact a much higher toll, particularly among those who may be malnourished or suffer from chronic ailments such as malaria and HIV.
In recent years researchers have also noted a much more virulent form of NTS, spreading across sub-Saharan Africa, that they’ve dubbed Invasive Non-Typhoidal Salmonella (iNTS).
Not only is it a multi-drug resistant strain, it is fatal in about 25% of those who contract it.
Today, we’ve a study that appears in Nature Genetics that links the Intracontinental spread and evolution of this invasive and severe form of Salmonella to the emergence and spread of HIV.
Intracontinental spread of human invasive Salmonella Typhimurium pathovariants in sub-Saharan Africa
Chinyere K Okoro,Robert A Kingsley,Thomas R Connor,Simon R Harris,Christopher M Parry,Manar N Al-Mashhadani,Samuel Kariuki,Chisomo L Msefula,Melita A Gordon,Elizabeth de Pinna,John Wain,Robert S Heyderman,Stephen Obaro,Pedro L Alonso,Inacio Mandomando,Calman A MacLennan, Milagritos D Tapia,Myron M Levine,Sharon M Tennant,Julian Parkhill & Gordon Dougan
Published online 30 September 2012
While the bulk of the study is behind a pay wall, the Abstract is available, as is this press release from the Wellcome Trust Sanger Institute.
New pathogen epidemic identified in sub-Saharan Africa

Researchers track the spread of human invasive non-Typhoidal Salmonella in sub-Saharan Africa
A new study out today (Sunday 30 September) reveals that the emergence and spread of a rapidly evolving invasive intestinal disease, that has a significant mortality rate (up to 45%) in infected people in sub-Saharan Africa, seems to have been potentiated by the HIV epidemic in Africa.
The team found that invasive non-Typhoidal Salmonella (iNTS) disease is caused by a new form of the bacteria Salmonella Typhimurium that has spread from two different focal hubs in Southern and Central Africa beginning 52 and 35 years ago, respectively. They also found that one of the major contributing factors for the successful spread of iNTS was the acquisition of genes that afford resistance to several front line drugs used to treat blood-borne infection such as iNTS.
iNTS is a blood-borne infection that kills approximately one of four people in sub-Saharan Africa who catch it. Yet, in the rest of the world, NTS is a leading cause of acute inflammatory diarrhoea that is self-limiting and tends to be fatal in less than 1 per cent of people infected. The disease is more severe in sub-Saharan Africa than the rest of the world because of factors such as malnutrition, co-infection with malaria or HIV and potentially the novel genotype of the Salmonella bacteria.
"The immune system susceptibility provided by HIV, malaria and malnutrition at a young age, may provide a population in sub-Saharan Africa that is large enough for this detrimental pathogen to enter, adapt, circulate and thrive," says Chinyere Okoro, joint first author from the Wellcome Trust Sanger Institute. "We used whole genome sequencing to define a novel lineage of Salmonella Typhimurium that is causing a previously unrecognised epidemic across the region. Its genetic makeup is evolving into a more typhoid like bacteria, able to efficiently spread around the human body"
<SNIP>
"There has been some evidence that this disease can be passed from human to human. Now the race is on to discover how NTS is actually transmitted in sub-Saharan Africa so that effective intervention strategies can be implemented."
And for more on all of this, here’s Debra McKenzie’s article for New Scientist.
HIV could be turning salmonella nastier
18:00 30 September 2012 by Debora MacKenzie
A nastier kind of salmonella infection has emerged alongside the HIV epidemic in Africa. The finding is the first evidence that HIV might be allowing new human pathogens to evolve in immunosuppressed people.